Topic Resources
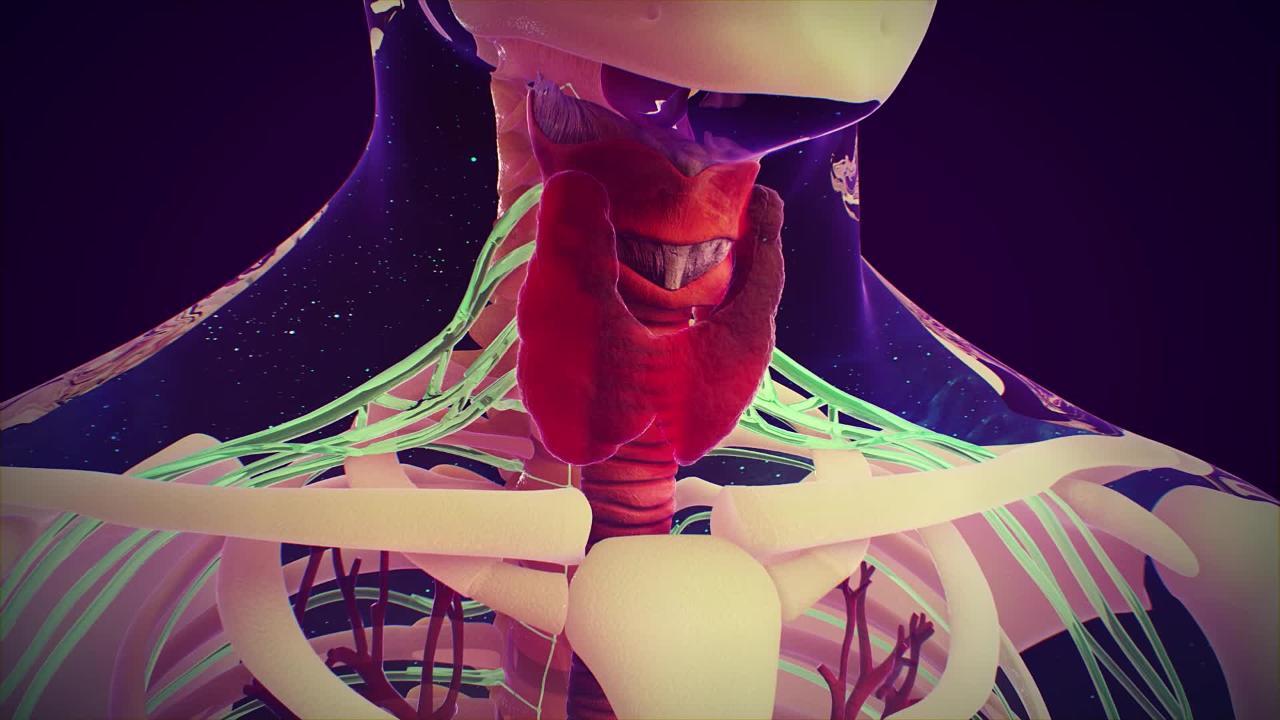
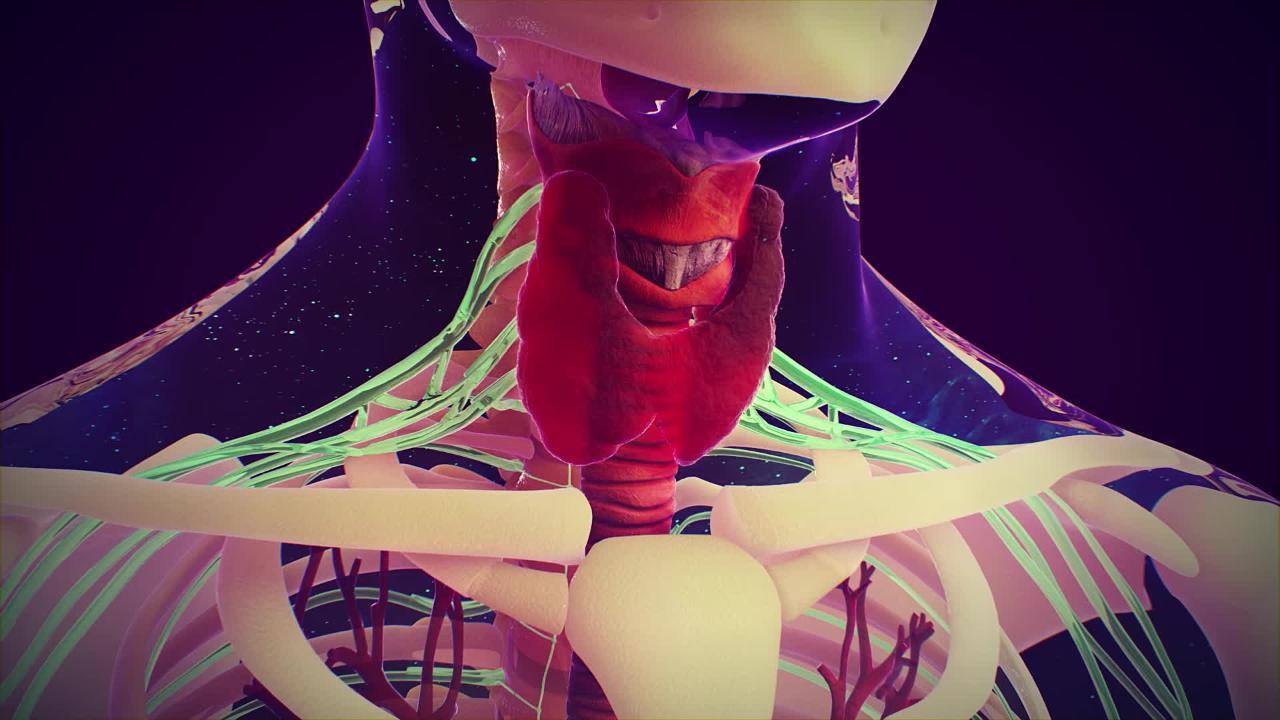
The cause of thyroid cancer is not known, but the thyroid gland is very sensitive to radiation, which may cause cancerous changes. Thyroid cancer is more common among people who were treated with radiation to the head, neck, or chest, most often for noncancerous (benign) conditions, when they were children (although radiation treatment for noncancerous conditions is no longer used).
(See also Overview of the Thyroid Gland.)
Thyroid nodules
Rather than causing the whole thyroid gland to enlarge, a cancer usually causes small growths (nodules) to develop within the thyroid. However, most thyroid nodules are not cancerous (malignant). A nodule is more likely to be cancerous if it
Is solid rather than filled with fluid (cystic)
Is not producing thyroid hormone
Is hard
Is growing quickly
Occurs in a man
Is associated with enlarged lymph nodes in the neck
A painless lump in the neck is usually the first sign of thyroid cancer. A larger cancer may press on nearby tissues in the neck, causing hoarseness, coughing, or difficulty breathing.
When doctors find a nodule in the thyroid gland, they request several tests. The first tests are generally thyroid function blood tests, in which the blood levels of thyroid-stimulating hormone (TSH), thyroid hormones T4 (thyroxine, or tetraiodothyronine) and T3 (triiodothyronine) are measured. Sometimes tests to detect antibodies to the thyroid are done.
If the blood tests show an overactive thyroid gland (hyperthyroidism), a thyroid scan is done to determine whether the nodule is producing thyroid hormones. Nodules that are producing hormones ("hot" nodules) are almost never cancerous. If the tests do not indicate hyperthyroidism or Hashimoto thyroiditis, or if the nodules are not “hot,” doctors usually do a fine-needle biopsy.
In a fine-needle biopsy, ultrasonography is done to image the nodule and then a sample of the nodule is removed through a small needle and then examined under a microscope. This procedure is not very painful, is carried out in the doctor’s office, and may involve the use of a local anesthetic as well as ultrasonography to guide needle placement.
Ultrasonography is also done to determine how large the nodule is, whether it is solid or filled with fluid, whether other nodules are present, and whether it has characteristics that are high risk for cancer.
Types of Thyroid Cancer
Thyroid cancers develop from different types of cells in the thyroid gland:
Follicular cells, which secrete thyroid hormone
Parafollicular (C) cells, which secrete the hormone calcitonin
Cancers that develop from follicular cells are more common. They include
Papillary thyroid cancer
Follicular thyroid cancer
Oncocytic thyroid cancer
Anaplastic thyroid cancer
Most thyroid cancers are papillary or follicular carcinomas. Oncocytic thyroid cancer is much less common. Papillary, follicular, and oncocytic cancers are typically slow growing. In contrast,anaplastic thyroid carcinomas grow more quickly.
Medullary thyroid cancer develops from parafollicular cells. It usually grows slowly but can spread to lymph nodes in the neck early in its development.
Papillary thyroid cancer
Papillary thyroid cancer is the most common type, accounting for 80 to 90% of all thyroid cancers. About 3 times as many women as men have papillary cancer. Papillary cancer is most common between the ages of 30 and 60 years but grows and spreads more quickly in older adults.
People who have received radiation treatment to the neck, usually for a noncancerous condition in infancy or childhood or for some other cancer in adulthood, are at greater risk of developing papillary cancer.
Papillary cancer grows within the thyroid gland but sometimes spreads (metastasizes) to nearby lymph nodes. If left untreated, papillary cancer may spread to more distant sites.
Papillary cancer is almost always curable.
For large nodules (particularly those larger than about 1.5 inches, or 4 centimeters), most or all of the thyroid gland is usually removed. Radioactive iodine is often given to destroy any remaining thyroid tissue or cancer. Thyroid hormone is also given in large doses to suppress the growth of any remaining thyroid tissue.
Nodules smaller than about 1.5 inches (4 centimeters) are removed along with the thyroid tissue immediately surrounding them (lobectomy and isthmusectomy), although many experts recommend removing the entire thyroid gland (thyroidectomy).
Doctors suggest active surveillance for people with very small papillary thyroid cancers that are not likely to spread to nearby tissues. During active surveillance, the person has an ultrasound examination of the thyroid every 6 months to detect any spread of the cancer.
Follicular thyroid cancer
Follicular thyroid cancer accounts for about 4% of all thyroid cancers and is more common among older adults. Follicular cancer is also more common in regions where iodine deficiency is more common.
Follicular thyroid cancer is more likely to spread to other organs in the body than papillary cancer. Follicular cancer tends to spread (metastasize) through the bloodstream, spreading cancerous cells to various parts of the body.
Treatment for follicular cancer requires surgically removing as much of the thyroid gland as possible and destroying any remaining thyroid tissue, including the metastases, if present, with radioactive iodine. It is usually curable, but less so than papillary cancer.
Oncocytic thyroid carcinoma
Oncocytic thyroid cancer (formerly called Hurthle cell carcinoma) accounts for about 3 to 5% of thyroid cancers. Oncocytic cancer is more likely to spread to other areas of the body. It also is more likely to have a poor prognosis. Treatment for oncocytic cancer requires surgically removing as much of the thyroid gland as possible.
Anaplastic thyroid cancer
Anaplastic thyroid cancer accounts for about 1% of thyroid cancers and is most common among older adults. It is slightly more common among older women. Many cases are due to a specific gene mutation. This cancer grows very quickly and usually causes a large, painful growth in the neck. It also tends to spread throughout the body.
Treatment of anaplastic cancer may include surgery to remove the thyroid gland (and sometimes the surrounding tissue), radiation therapy, chemotherapy, or a combination. Many people with anaplastic cancer die within 1 year, even with treatment. However, newer cancer drugs, including medications called checkpoint inhibitors, show promise of improving prognosis for people with anaplastic thyroid cancer. Radioactive iodine is not helpful in the treatment of this type of cancer.
Medullary thyroid cancer
About 4% of thyroid cancers are a medullary thyroid cancer that begins in the thyroid gland but in a different type of cell than that which produces thyroid hormone. The origin of this cancer is the C-cell, which is normally dispersed throughout the thyroid and secretes the hormone calcitonin, which helps control the level of calcium in the bloodstream. Medullary thyroid cancer produces excessive amounts of calcitonin. Because medullary thyroid cancer can also produce other hormones, it can cause unusual symptoms.
This cancer tends to spread (metastasize) through the lymphatic vessels to the lymph nodes and through the blood to the liver, lungs, and bones. Medullary thyroid cancer can develop along with other types of endocrine cancers in what is called multiple endocrine neoplasia syndrome.
Treatment requires surgically removing the thyroid gland. Additional surgery may be needed to determine whether the cancer has spread to the lymph nodes. Radioactive iodine is not used in the treatment of this type of cancer. More than two thirds of people whose medullary thyroid cancer is part of multiple endocrine neoplasia syndrome are cured.
Because medullary thyroid cancer is often familial, people undergo genetic testing to identify the gene mutation causing the cancer. If a mutation is identified, doctors may recommend further testing for family members, and some family members may even have their thyroid removed before cancer can develop.