Topic Resources
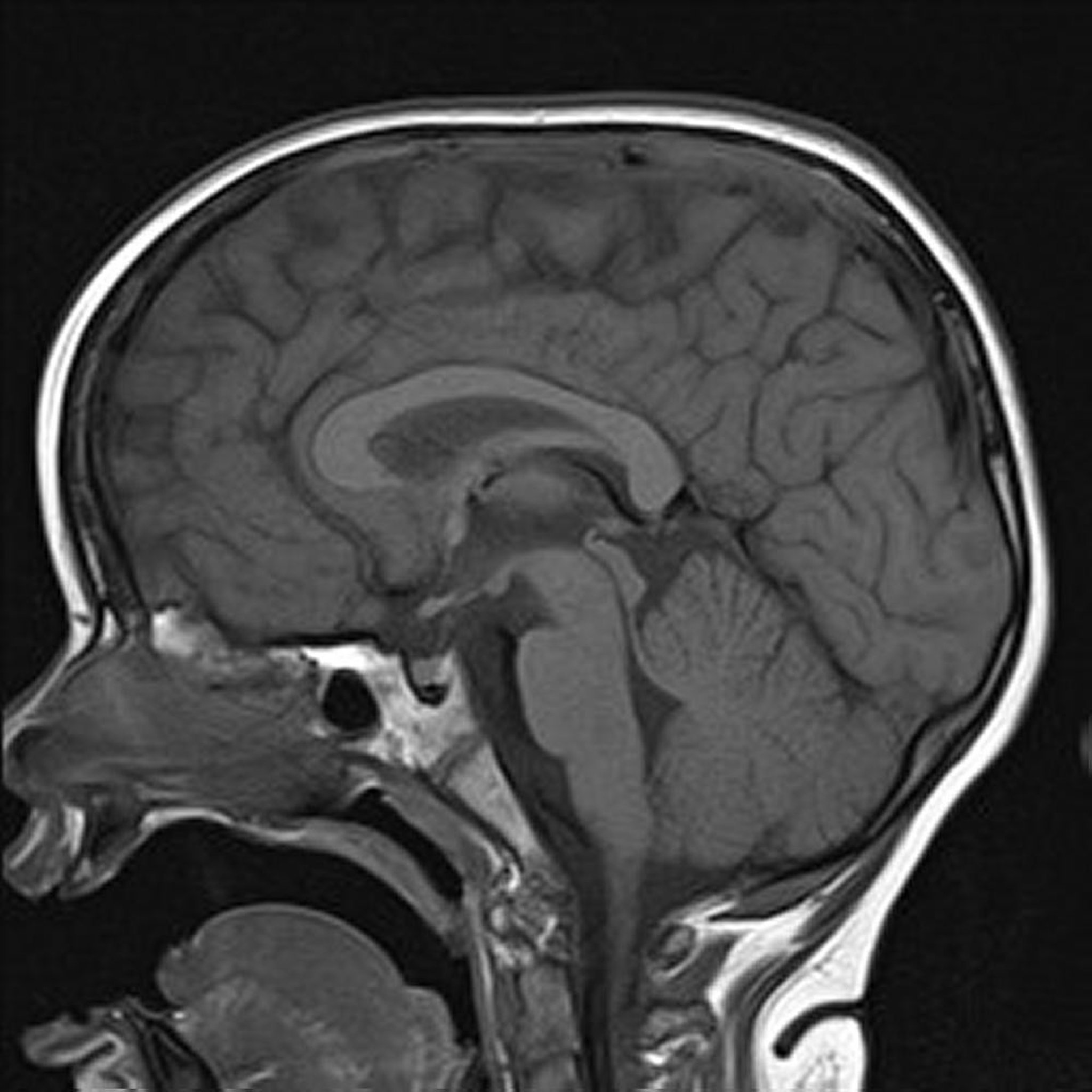
Image courtesy of Hakan Ilaslan, MD.
Image courtesy of Hakan Ilaslan, MD.
Image courtesy of Hakan Ilaslan, MD.
MRI uses magnetic fields and radio waves to produce images of thin slices of tissues (tomographic images). Normally, protons within tissues spin to produce tiny magnetic fields that are randomly aligned. When surrounded by the strong magnetic field of an MRI device, the magnetic axes align along that field. A radiofrequency pulse is then applied, causing the axes of many protons to momentarily align against the field in a high-energy state. After the pulse, protons relax and resume their baseline alignment within the magnetic field of the MRI device. The magnitude and rate of energy release that occurs as the protons resume this alignment (T1 relaxation) and as they wobble (precess) during the process (T2 relaxation) are recorded as spatially localized signal intensities by a coil (antenna) built within the MRI device. Computer algorithms analyze these signals and produce detailed anatomic images.
The relative signal intensity (brightness) of tissues in an MRI image is determined by factors such as
The radiofrequency pulse and gradient waveforms used to obtain the image
Intrinsic T1 and T2 characteristics of different tissues
The proton density of different tissues
By controlling the radiofrequency pulse and gradient waveforms, computer programs produce specific pulse sequences that determine how an image is obtained (weighted) and how various tissues appear. Images can be
T1-weighted
T2-weighted
Proton density–weighted
For example, fat appears bright (high signal intensity) on T1-weighted images and relatively dark (low signal intensity) on T2-weighted images; water and fluids appear relatively dark on T1-weighted images and bright on T2-weighted images. T1-weighted images optimally show normal soft-tissue anatomy and fat (eg, to confirm a fat-containing mass). T2-weighted images optimally show fluid and abnormalities (eg, tumors, inflammation, trauma). In practice, T1- and T2-weighted images provide complementary information, so both are important for characterizing abnormalities.
Recently introduced high-resolution MRI scanners increase image quality and diagnostic accuracy and produce a wide variety of additional pulse sequences to further characterize tissues and tumors.
Uses of MRI
MRI is preferred to CT when soft-tissue contrast resolution must be highly detailed (eg, to evaluate intracranial or spinal cord abnormalities, inflammation, trauma, suspected musculoskeletal tumors, or internal joint derangement). MRI is also useful for the following:
Vascular imaging: Magnetic resonance angiography (MRA) is used to image arteries with good diagnostic accuracy and is less invasive than conventional angiography. A gadolinium contrast agent is sometimes used. MRA can be used to image the thoracic and abdominal aorta and arteries of the brain, neck, abdominal organs, kidneys, and lower extremities. Venous imaging (magnetic resonance venography, or MRV) provides the best images of venous abnormalities, including thrombosis and anomalies.
Hepatic and biliary tract abnormalities: Magnetic resonance cholangiopancreatography (MRCP) is particularly valuable as a noninvasive, highly accurate method of imaging the biliary and pancreatic duct systems.
Masses in the female reproductive organs: MRI supplements ultrasonography to further characterize adnexal masses and to stage uterine tumors.
Certain fractures: For example, MRI can provide accurate images of hip fractures in patients with osteopenia.
Bone marrow infiltration and bone metastases: MRI is particularly useful for evaluating patients with positive bone scintigraphy and normal x-rays and for characterizing bone marrow abnormalities as metastases versus nonmalignant lesions.
MRI can also be substituted for CT with contrast in patients with a high risk of reactions to iodinated contrast agents.
Contrast agents
With MRI, contrast agents are often used to highlight vascular structures and to help characterize inflammation and tumors.
The most commonly used agents are gadolinium derivatives, which have magnetic properties that affect proton relaxation times. MRI of intra-articular structures may include injection of a diluted gadolinium derivative into a joint.
Variations of MRI
Diffusion (diffusion-weighted) MRI
Signal intensities are related to diffusion of water molecules in tissue. This type of MRI can be used
To detect early cerebral ischemia and infarction
To detect white matter disease of the brain
To differentiate abscess from a cystic tumor
To stage various tumors such as non–small cell lung cancer
Echo planar imaging
This ultrafast technique (images obtained in < 1 second) is used for diffusion, perfusion, and functional imaging of the brain and heart. Its potential advantages include showing brain and heart activity and reducing motion artifacts. However, its use is limited because it requires special technical hardware and is more sensitive to various artifacts than conventional MRI.
Functional MRI
Functional MRI is used to assess brain activity by location.
In the most common type, the brain is scanned at low resolution very frequently (eg, every 2 to 3 seconds). The change in oxygenated hemoglobin can be discerned and used to estimate metabolic activity of different parts of the brain.
Researchers sometimes do functional MRI while subjects do different cognitive tasks (eg, solve a math equation); the metabolically active parts of the brain are presumed to be the structures most involved in that particular task. Correlating brain function and anatomy this way is called brain mapping.
Functional MRI can be used in both research and clinical settings. It is especially helpful clinically in mapping of motor or language cortices (ie, cortical areas that when removed result in deficits in sensory processing, motor function, or language processing) in patients with intracranial abnormalities such as tumors and arteriovenous malformations for whom surgery is being planned. It is also used increasingly to plan epilepsy surgery.
Gradient echo imaging
Gradient echo is a pulse sequence that can be used for fast imaging of moving blood and cerebrospinal fluid (eg, in MRA). Because this technique is fast, it can reduce motion artifacts (eg, blurring) during imaging that requires patients to hold their breath (eg, during imaging of cardiac, pulmonary, and abdominal structures).
Magnetic resonance spectroscopy (MRS)
MRS combines the information obtained by MRI (mainly based on water and fat content of tissues) with that of nuclear magnetic resonance (NMR). NMR provides information about tissue metabolites and biochemical abnormalities; this information can help differentiate certain types of tumors and other abnormalities.
Magnetic resonance enterography
Magnetic resonance enterography has become popular, especially for follow-up imaging of children with known inflammatory conditions of the small bowel.
Because magnetic resonance enterography does not require ionizing radiation, it has an advantage over CT enterography.
Perfusion MRI
Perfusion MRI is a method of assessing relative cerebral blood flow. It can be used to detect
Areas of ischemia during imaging for stroke
Areas of increased vascularity that can indicate tumors
This information can help direct biopsy.
Positron emission tomography (PET)–MRI
PET-MRI combines functional PET with whole-body MRI. T1-weighted and short T1 inversion recovery (STIR) sequences are frequently used. This method is new and is available in only a few major medical centers.
Disadvantages of MRI
MRI is relatively expensive, requires longer imaging times than CT and may not be immediately available in all areas.
Other disadvantages include problems related to
The magnetic field
Patient claustrophobia
Contrast reactions
Magnetic field
MRI is relatively contraindicated in patients with implanted materials that can be affected by powerful magnetic fields. These materials include
Ferromagnetic metal (ie, containing iron)
Magnetically activated or electronically controlled medical devices (eg, pacemakers, implantable cardioverter defibrillators, cochlear implants)
Nonferromagnetic electrical wires or materials (eg, pacemaker wires, certain pulmonary artery catheters)
Ferromagnetic material may be displaced by the strong magnetic field, injuring a nearby organ; for example, displacement of vascular clips can result in hemorrhage. Displacement is more likely if the material has been in place < 6 weeks (before scar tissue forms). Ferromagnetic material can also cause imaging artifacts.
Magnetically activated medical devices may malfunction when exposed to magnetic fields.
Magnetic fields may induce current in any conductive materials strong enough to produce enough heat to burn tissues.
Whether a specific device is compatible with MRI depends on the type of device, its components, and its manufacturer (see MRIsafety.com). Patients with an implantable device should not be placed in the MRI magnetic field until examiners are sure that MRI is safe with such a device in place. Also, MRI machines with different magnetic field strengths have different effects on materials, so safety in one machine does not ensure safety in another.
The MRI magnetic field is very strong and may always be on. Thus, a ferromagnetic object (eg, an oxygen tank, a metal pole) at the entrance of the scanning room may be pulled into the magnet bore at high velocity and injure anyone in its path. The only way to separate the object from the magnet may be to turn off (quench) the magnetic field.
Claustrophobia
The imaging tube of an MRI machine is a tight, enclosed space that can trigger claustrophobia even in patients without preexisting phobias or anxiety. Also, some patients with obesity do not fit on the table or within the machine. Premedication with an antianxiety medication (eg, alprazolam or lorazepam 1 to 2 mg orally) 15 to 30 minutes before scanning is effective for most anxious patients. The imaging tube of an MRI machine is a tight, enclosed space that can trigger claustrophobia even in patients without preexisting phobias or anxiety. Also, some patients with obesity do not fit on the table or within the machine. Premedication with an antianxiety medication (eg, alprazolam or lorazepam 1 to 2 mg orally) 15 to 30 minutes before scanning is effective for most anxious patients.
MRI scanners with an open side can be used for patients with claustrophobia (or those with severe obesity). Images obtained during open MRI may be inferior to those of enclosed scanners depending on the field strength of the magnet, but they are usually sufficient for making a diagnosis.
Patients should be warned that the MRI machine makes loud, banging noises during scanning.
Contrast reactions
Gadolinium-based contrast agents injected IV can cause headache, nausea, pain, and distortion of taste, as well as sensation of cold at the injection site.
Serious contrast reactions are rare and much less common than with iodinated contrast agents.
However, nephrogenic systemic fibrosis (NSF) has been reported in a small number of patients with advanced chronic kidney disease, and most of these cases are linked to group I gadolinium-based contrast media (GBCM). NSF is a rare but life-threatening disorder that involves fibrosis of the skin, blood vessels, and internal organs, resulting in severe disability or death. Group I GBCM is no longer advertised in the United States or Europe (see European Medicines Agency, November 2009 press release).
The likelihood of developing NSF or nephrotoxicity is extremely low in patients who received group II GBCM, even in high-risk patients. The consensus statement from the American College of Radiology and the National Kidney Foundation indicates that kidney function screening is not mandatory for any Group II GBCM (1). Gadolinium-based contrast agents should be used only when necessary and at the lowest possible dose.
Reference
1. Weinreb JC, Rodby RA, Yee J, et al: Use of Intravenous Gadolinium-based Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation. Radiology 298(1):28-35, 2021. doi:10.1148/radiol.2020202903
Drugs Mentioned In This Article