- Overview of Coronary Artery Disease
- Angina Pectoris
- Microvascular Angina
- Vasospastic Angina
- Overview of Acute Coronary Syndromes (ACS)
- Unstable Angina
- Acute Myocardial Infarction (MI)
- Complications of Acute Coronary Syndromes
- Medications for Acute Coronary Syndromes
- Overview of Revascularization for Acute Coronary Syndromes
- Percutaneous Coronary Interventions (PCI)
- Coronary Artery Bypass Grafting (CABG)
Topic Resources
Coronary artery bypass grafting (CABG) involves bypassing native coronary arteries that have high-grade stenosis or occlusion not amenable to angioplasty with stent insertion. Indications are changing as percutaneous interventions are being increasingly used.
Traditional CABG Procedure
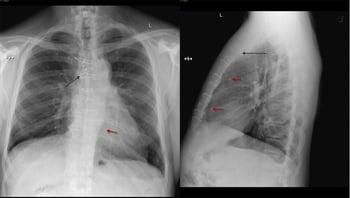
Traditional coronary artery bypass grafting involves thoracotomy via a midline (median) sternotomy. A heart-lung machine is used to establish cardiopulmonary bypass (CPB), allowing the heart to be stopped and emptied of blood to maximize operative exposure and facilitate vessel anastomosis; stopping the heart also markedly decreases myocardial oxygen demand.
Before initiation of CPB, the patient is given a very high dose of heparin to prevent clotting in the bypass circuit. Then the aorta is cross-clamped and the heart is stopped by injection of a cardioplegic solution (crystalloid or more commonly blood-based) that also contains substances that help myocardial cells tolerate ischemia and reperfusion. The cardioplegic solution and the heart are sometimes cooled slightly to enhance tolerance of ischemia; the patient’s body is cooled via the CPB machine for similar reasons.Before initiation of CPB, the patient is given a very high dose of heparin to prevent clotting in the bypass circuit. Then the aorta is cross-clamped and the heart is stopped by injection of a cardioplegic solution (crystalloid or more commonly blood-based) that also contains substances that help myocardial cells tolerate ischemia and reperfusion. The cardioplegic solution and the heart are sometimes cooled slightly to enhance tolerance of ischemia; the patient’s body is cooled via the CPB machine for similar reasons.
The left internal mammary artery is typically used as a pedicled graft to the left anterior descending coronary artery. Other grafts consist of segments of saphenous vein removed from the leg. Occasionally, the right internal mammary artery or radial artery from the nondominant arm can be used.
On completion of the vascular anastomoses, the aorta is unclamped, allowing the coronary arteries to be perfused by oxygenated blood, which typically restores cardiac activity. Heparin anticoagulation is reversed by giving protamine. On completion of the vascular anastomoses, the aorta is unclamped, allowing the coronary arteries to be perfused by oxygenated blood, which typically restores cardiac activity. Heparin anticoagulation is reversed by giving protamine.
Despite cardioprotective measures, stopping the heart is not without consequences. During reperfusion, myocardial dysfunction is common and can lead to bradycardia, arrhythmias (eg, ventricular fibrillation), and low cardiac output; these events are treated by standard measures, such as pacing, defibrillation, and inotropic drugs.
Typically, hospital stays are 4 to 5 days unless prolonged by complications or concomitant illnesses.
Complications of coronary artery bypass grafting
Complications and disadvantages of traditional CABG involve mainly
Sternotomy
Cardiopulmonary bypass
Median sternotomy is surprisingly well tolerated; however, healing takes 4 to 6 weeks. Also, wound infections occasionally cause mediastinitis or sternal osteomyelitis, which can be difficult to treat.
CPB causes several major complications, including
Bleeding
Organ dysfunction, including neuropsychiatric effects
Stroke
Post-CPB bleeding is a common problem caused by various factors, including hemodilution, heparin use, platelet dysfunction due to exposure to the bypass pump, is a common problem caused by various factors, including hemodilution, heparin use, platelet dysfunction due to exposure to the bypass pump,disseminated intravascular coagulation, and induced hypothermia.
Organ dysfunction may result from a systemic inflammatory response caused by the CPB machine (probably due to exposure of blood components to the foreign material of the bypass circuit); this response can cause organ dysfunction in any system (eg, pulmonary, renal, brain, gastrointestinal). Aortic cannulation, cross-clamping, and release can trigger release of emboli, causing stroke. For patients with a normal-sized heart, no history of MI, good ventricular function, and no additional risk factors, risk is 1 to 2% for stroke.
Post-CPB neuropsychiatric effects may develop, probably secondary to microemboli, in about 25 to 30% (1). Cognitive or behavioral changes are more prevalent in older patients, prompting suspicion that these changes are most likely due to diminished "neuronal reserve," making older patients more susceptible to minor injuries incurred during cardiopulmonary bypass. Dysfunction ranges from mild to severe and may persist for weeks to years. It is not clear that using a beating heart technique (off-pump CABG, which uses no cardiopulmonary bypass) decreases long-term risks of neuropsychiatric effects.
Other common complications of CABG include
Arrhythmias
Focal myocardial ischemia
Global myocardial ischemia
Perioperative myocardial infarction occurs in about 1% of patients. For patients with a normal-sized heart, no history of MI, good ventricular function, and no additional risk factors, risk is < 5% for perioperative MI. Atrial fibrillation occurs in 15 to 40% of patients, typically 2 to 4 days after surgery. Beta-blockers (including sotalol) and amiodarone appear to reduce the likelihood of the development of atrial arrhythmias after cardiac surgery. Nonsustained ventricular tachycardia may occur in up to 50% of patients.occurs in 15 to 40% of patients, typically 2 to 4 days after surgery. Beta-blockers (including sotalol) and amiodarone appear to reduce the likelihood of the development of atrial arrhythmias after cardiac surgery. Nonsustained ventricular tachycardia may occur in up to 50% of patients.
Mortality depends mainly on patients’ underlying health; operator and institutional experience (ie, number of annual procedures) also is important. In an experienced program, periprocedural mortality in otherwise healthy patients is typically < 1 to 3% (2). For patients with a normal-sized heart, no history of MI, good ventricular function, and no additional risk factors, risk is ≤ 1% for mortality.
Risks of stroke, perioperative myocardial infarction, and mortality increase with age, poor LV function, and presence of underlying disease.
A simple calculator can categorize risks associated with CABG into three groups (low, intermediate, high). The Society of Thoracic Surgeons (STS) publishes a more advanced Short-Term/Operative Risk Calculator used to assess risk of operative mortality, major morbidity, and complications after most cardiac procedure categories in the Adult Cardiac Surgery Database (ACSD) (eg, stroke, renal failure).
Traditional CABG procedure references
1. Kulik A, Ruel M, Jneid H, et al: Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation 131(10):927–964, 2015. doi:10.1161/CIR.0000000000000182
2. Peterson ED, Coombs LP, DeLong ER, Haan CK, Ferguson TB: Procedural volume as a marker of quality for CABG surgery. JAMA 291(2):195–201, 2004. doi:10.1001/jama.291.2.195
Alternative CABG Procedures
Alternative techniques seek to limit the complications of traditional coronary artery bypass grafting by
Avoiding cardiopulmonary bypass (off-pump CABG)
Avoiding median sternotomy (minimally invasive CABG)
Both
Off-pump CABG
Cardiopulmonary bypass can be avoided in select patients by using techniques that allow the surgeon to revascularize the beating heart. Various devices and methods stabilize a portion of the myocardium, holding the operative site relatively motionless.
Off-pump CABG procedures are more commonly done through small parasternal or intercostal incisions (minimally invasive CABG), sometimes with endoscopy or even robotic assistance, but they may be done through a traditional median sternotomy, which provides better operative exposure.
Allowing the heart to beat means that the myocardium requires more oxygen than when CPB is used. Thus, the heart is sensitive to the interruption of blood flow necessitated while the vascular anastomosis is done; this interruption can cause ischemia or infarction in the myocardium supplied by the affected vessel. Some surgeons place a temporary coronary artery shunt to provide distal perfusion.
Off-pump CABG is technically more challenging but may be appropriate in patients who have significant aortic calcifications that causes manipulation of the aorta to be of higher risk. Compared to on-pump procedures, off-pump CABG is associated with increased need for revascularization at one year.
Minimally invasive CABG
The minimally invasive CABG technique is somewhat more difficult to do and may not be suitable when multiple bypass grafts, particularly those involving vessels behind the heart, are required. Transfusion requirements, length of stay, and costs are typically less with off-pump CABG, but in some studies, the rate of the more serious complications of death, myocardial infarction, and stroke are similar to that of CABG using CPB. Thus, the theoretic advantages of avoiding CPB do not seem to have been fully realized.
Minimally invasive CABG is usually done off-pump but may be done using CPB. In such cases, CPB is done endovascularly using special catheters inserted into the arterial and venous systems; the aorta is occluded by a balloon at the end of the aortic catheter rather than an external clamp. Although avoiding median sternotomy complications, this technique otherwise has similar rates of mortality and major perioperative complications as conventional techniques (1).
Alternative CABG procedures reference
1. Teman NR, Hawkins RB, Charles EJ, et al. Minimally Invasive vs Open Coronary Surgery: A Multi-Institutional Analysis of Cost and Outcomes. Ann Thorac Surg 2021;111(5):1478-1484. doi:10.1016/j.athoracsur.2020.06.136
Drugs Mentioned In This Article