Systemic lupus erythematosus is a chronic systemic rheumatic disease that can involve joints, kidneys, skin, mucous membranes, and blood vessel walls.
Problems in the joints, nervous system, blood, skin, kidneys, gastrointestinal tract, lungs, and other tissues and organs can develop.
Blood tests and sometimes other tests are done to make the diagnosis.
All people with lupus need hydroxychloroquine, and people with lupus that is continuing to cause damage (active lupus) also need corticosteroids and other medications that suppress the immune system.All people with lupus need hydroxychloroquine, and people with lupus that is continuing to cause damage (active lupus) also need corticosteroids and other medications that suppress the immune system.
Women, usually women of child-bearing age, have a greater risk of developing systemic lupus erythematosus (lupus) than men. However, children (mostly girls), older men and women, and even newborns can also be affected. Lupus occurs in all parts of the world and is more common and severe among Black people and Asian people than White people.
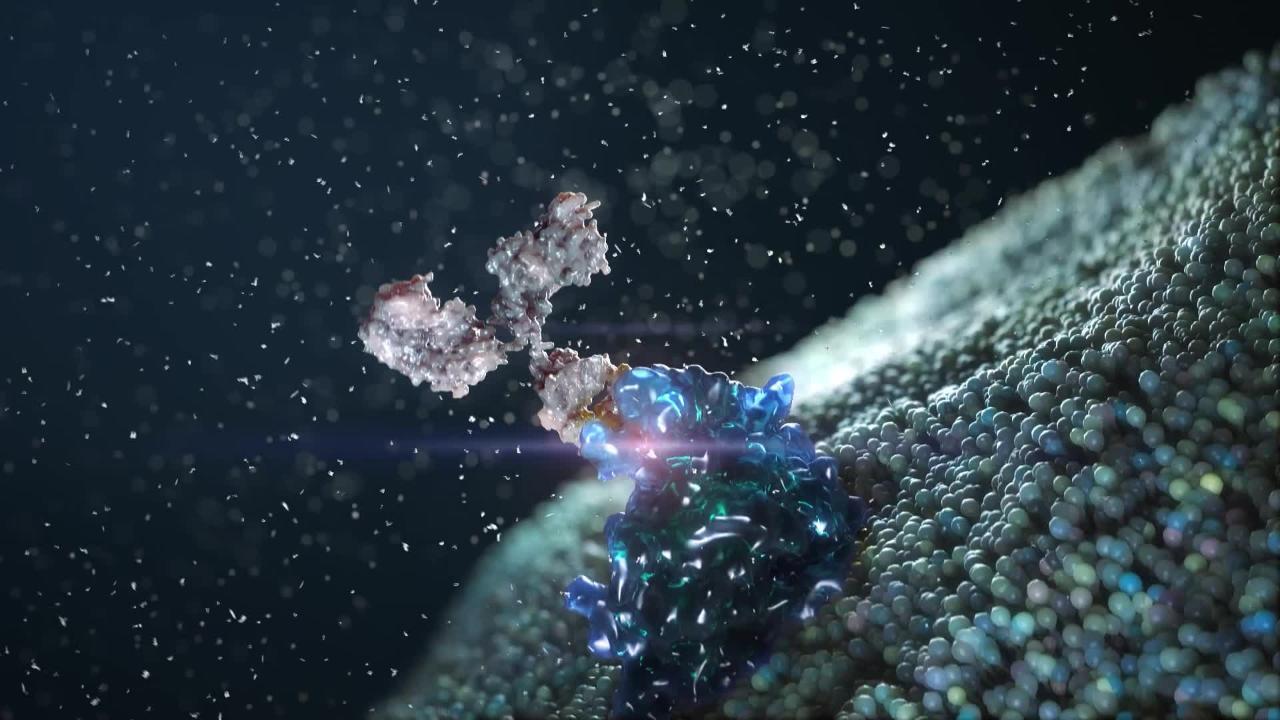
The cause of lupus is usually not known, but it is thought to be an autoimmune disorder. In an autoimmune disorder, antibodies or cells produced by the body attack the body’s own tissues. Occasionally, the use of certain medications (such as hydralazine and procainamide, which are used to treat heart conditions, and isoniazid, which is used to treat tuberculosis) can cause lupus. Medication-induced lupus usually disappears after the medication is stopped., antibodies or cells produced by the body attack the body’s own tissues. Occasionally, the use of certain medications (such as hydralazine and procainamide, which are used to treat heart conditions, and isoniazid, which is used to treat tuberculosis) can cause lupus. Medication-induced lupus usually disappears after the medication is stopped.
When lupus is actively causing symptoms, it is known as a flare-up. Flare-ups can be triggered by sun exposure, infection, surgery, or pregnancy.
Cutaneous lupus
Some forms of lupus predominantly affect the skin.
Discoid lupus erythematosus (DLE) is a form of lupus that affects only the skin.
In DLE, raised, round, red rashes occur, sometimes progressing to some loss of the skin with scarring and hair loss in affected areas. The rash clusters on light-exposed areas of the skin, such as the face, scalp, and ears. Sometimes a rash or sores also affect the mucous membranes, especially in the mouth.
Some people who have DLE also develop manifestations of systemic lupus erythematosus such as joint, kidney, and brain problems.
© Springer Science+Business Media
Subacute cutaneous lupus erythematosus (SCLE) is a form of lupus that mostly affects the skin.
In SCLE, various, widespread rashes occur. They may come and go and may worsen with exposure to sunlight. Red and ring-shaped or psoriasis–like patches may form on the arms, face, and trunk.
SCLE differs from DLE because SCLE rarely causes scarring.
Some people who have SCLE may develop systemic lupus erythematosus.
Symptoms of Lupus
Symptoms of lupus vary greatly from person to person. Symptoms may begin suddenly with fever, resembling a sudden infection. Or symptoms may develop gradually over months or years with episodes (called flare-ups) of fever, feeling unwell, or any of the symptoms discussed below alternating with periods when symptoms are absent or minimal. Most people with lupus have mild symptoms affecting mostly the skin and joints. However, symptoms may affect any organ system.
Joint problems
Joint symptoms, ranging from intermittent joint pains (arthralgias) to sudden inflammation of multiple joints (acute polyarthritis), occur in approximately 90% of people and may exist for years before other symptoms appear. In long-standing disease, marked joint looseness and deformity called Jaccoud arthritis or Jaccoud arthropathy may occur, but it is rare. However, most polyarthritis is intermittent and usually does not damage the joints.
Skin and mucous membrane problems
Skin problems include a raised, red rash across the nose and cheeks (called a malar rash or butterfly rash), raised bumps or patches of thin skin, and flat or raised red areas on exposed areas of the face and neck, upper chest, and elbows. Blisters and skin ulcers (sores) are rare, but ulcers do commonly occur on mucous membranes, particularly on the roof of the mouth, on the inside of the cheeks, on the gums, and inside the nose.
Generalized or patchy loss of hair (alopecia) is common during flare-ups.
Mottled red areas on the sides of the palms and up the fingers, redness and swelling around the nails, and flat, reddish purple blotches between the knuckles on the inner surfaces of the fingers also may occur. Purplish spots (purpura) may occur because of bleeding in the skin as a result of low platelet levels in the blood.
Long-lasting rashes resulting from exposure to sunlight (photosensitivity) occur in some people with lupus, particularly people who have light skin.
© Springer Science+Business Media
© Springer Science+Business Media
People with lupus who have Raynaud syndrome have very pale or bluish fingers and toes when they are exposed to cold.
Lung problems
It is common for people with lupus to feel pain when breathing deeply. The pain is due to recurring inflammation of the sac around the lungs (pleurisy), with or without fluid (effusion) inside this sac.
Inflammation of the lungs (lupus pneumonitis), resulting in breathlessness, is rare, although minor abnormalities in lung function are common.
Life-threatening bleeding into the lungs may rarely occur. Blockage of arteries in the lung caused by blood clots (thrombosis) can also occur.
Heart problems
People with lupus may have chest pain due to inflammation of the sac around the heart (pericarditis). More serious but rare effects on the heart are inflammation of the walls of the coronary arteries (coronary artery vasculitis), which can lead to angina, and inflammation of the heart muscle (myocarditis), which can lead to heart failure. The valves of the heart can rarely be involved and may need to be surgically repaired. People are at increased risk of coronary artery disease.
An infant whose mother has lupus and has a certain type of antibody (anti-Ro/SSA antibody) can be born with heart block.
Lymph node and spleen problems
Widespread enlargement of the lymph nodes is common, particularly among children, young adults, and African American people of all ages.
Enlargement of the spleen (splenomegaly) can occur.
Nervous system problems
Involvement of the brain (neuropsychiatric lupus) can cause headaches, mild impairment of thinking, personality changes, stroke, seizures, severe mental disorders (psychoses), or a condition in which a number of physical changes may occur in the brain.
The nerves in the spinal cord and elsewhere in the body also may be damaged.
Kidney problems
Kidney involvement may be minor and without symptoms or may be progressive and fatal. People may develop kidney failure that requires dialysis. The kidneys can be affected at any time and may be the only organ affected by lupus (called lupus nephritis).
Kidney impairment commonly causes high blood pressure and protein in the urine that leads to swelling (edema) in the legs.
Blood problems
The numbers of red blood cells, white blood cells, and platelets may decrease. Platelets assist in blood clotting, so if these numbers decrease greatly, bleeding may occur.
Also, and for other reasons, the blood may clot too easily, which accounts for some of the problems that can affect other organs (such as strokes and blood clots to the lungs or repeated miscarriages).
Gastrointestinal tract problems
People may have nausea, diarrhea, and vague abdominal discomfort. The occurrence of these symptoms may be the forewarning of a flare-up.
Impairment of blood supply to various parts of the gastrointestinal tract may result in more severe abdominal pain, damage to the liver or pancreas (pancreatitis), or a blockage or hole (perforation) of the gastrointestinal tract.
Pregnancy problems
Pregnant women have a higher-than-normal risk of multiple, late miscarriages and stillbirth. Flare-ups are common during pregnancy and especially immediately after delivery (see also Systemic Lupus Erythematosus in pregnancy).
Doctors advise women not to conceive if their lupus has not been controlled during the prior 6 to 12 months.
Diagnosis of Lupus
A doctor's examination
Laboratory tests
Doctors suspect lupus mainly on the basis of the person’s symptoms, particularly in a young woman, and on the results of a thorough physical examination.
To help confirm the diagnosis, doctors do several laboratory tests. Although there is no single laboratory test that confirms the diagnosis of lupus, doctors do these tests to rule out other systemic rheumatic diseases. Doctors then base the diagnosis of lupus on all of the information they gather, including symptoms, physical examination results, and all test results. Doctors use this information to help them determine whether people meet specific, established criteria that are used to confirm lupus. Nonetheless, because of the wide range of symptoms, distinguishing lupus from similar diseases and making the diagnosis can be challenging.
Laboratory tests
Although blood test results can help doctors diagnose lupus, they alone cannot confirm a definite diagnosis of lupus because sometimes the abnormalities they detect are present in healthy people or in people who have other disorders.
A blood test can detect antinuclear antibodies (ANA), which are present in almost all people who have lupus. However, these antibodies also occur in other diseases. Therefore, if ANA are detected, a test for antibodies to double-stranded DNA as well as a test for other autoimmune antibodies (autoantibodies) are done. A high level of these antibodies to DNA strongly supports the diagnosis of lupus, but not all people who have lupus have these antibodies.
Other blood tests, such as measuring the level of complement proteins (proteins with various immune functions, such as killing bacteria), are also done and can help monitor disease activity and determine the need for treatment.
Women with lupus who have repeated miscarriages or have had problems with blood clots should be tested for antiphospholipid antibodies. This is an important test when planning contraceptive methods or pregnancy. This blood test, which detects antibodies to phospholipids, can also help identify people at risk of repeated blood clots. Women with positive antibodies to phospholipids should not take estrogen-containing oral contraceptives and should choose other methods of contraception.
Blood tests can also indicate a low red blood cell count (anemia), a low white blood cell count, or a low platelet count. People who have anemia undergo a direct Coombs test. This test is used to detect increased amounts of certain antibodies that are attached to the surface of red blood cells and can destroy red blood cells, causing anemia.
Additional laboratory tests are done to detect the presence of protein or red blood cells in the urine (urinalysis) or an elevation of creatinine in the blood. These findings indicate kidney inflammation of the filtering structure in the kidneys (glomeruli), a condition referred to as glomerulonephritis. Sometimes a kidney biopsy (removal of tissue for examination and testing) is done to help the doctor plan treatment. People who have lupus should be tested frequently for kidney damage even if they have no symptoms (see Kidney Function Tests).
Treatment of Lupus
Hydroxychloroquine (an antimalarial) for all affected peopleHydroxychloroquine (an antimalarial) for all affected people
Nonsteroidal anti-inflammatory drugs (NSAIDs) and antimalarials for mild disease
NSAIDs, antimalarials, sometimes corticosteroids, and sometimes belimumab for mild to moderate diseaseNSAIDs, antimalarials, sometimes corticosteroids, and sometimes belimumab for mild to moderate disease
Corticosteroids, other immunosuppressants, and antimalarials for severe disease
Treatment of lupus depends on which organs are affected and how active the inflammation is. The severity of organ damage in lupus is not necessarily the same as the activity of inflammation. For example, organs may be permanently damaged and scarred from lupus that caused inflammation in the past. Such damage may be referred to as “severe,” even if the lupus is not active (that is, it is not causing any inflammation or any further damage at this time). The goal of treatment is to decrease the activity of lupus—that is, to decrease inflammation, which in turn should prevent new or further damage.
The antimalarial hydroxychloroquine is given by mouth to all people who have lupus regardless of whether their disease is mild or severe because it decreases flare-ups and decreases their risk of death. It may also reduce problems in people whose blood clots too easily or too often. However, hydroxychloroquine is not given to people who have a negative side effect. It may or may not be given to people who have The antimalarial hydroxychloroquine is given by mouth to all people who have lupus regardless of whether their disease is mild or severe because it decreases flare-ups and decreases their risk of death. It may also reduce problems in people whose blood clots too easily or too often. However, hydroxychloroquine is not given to people who have a negative side effect. It may or may not be given to people who haveG6PD deficiency (G6PD is an enzyme that protects red blood cells from certain toxic chemicals) because it can rapidly destroy red blood cells.
People who take hydroxychloroquine should have a yearly eye examination because this medication slightly increases the risk of damage to the back of the eye when it is taken for many years. People who take hydroxychloroquine should have a yearly eye examination because this medication slightly increases the risk of damage to the back of the eye when it is taken for many years.
Mild to moderate lupus
If lupus is not very active, causing mild joint or skin symptoms, treatment may not need to be intensive. Nonsteroidal anti-inflammatory drugs (NSAIDs) often can relieve joint pain but should usually not be taken for long periods of time uninterrupted. Antimalarials, such as hydroxychloroquine, chloroquine, or quinacrine, help relieve skin and joint symptoms and reduce the frequency of flare-ups. (NSAIDs) often can relieve joint pain but should usually not be taken for long periods of time uninterrupted. Antimalarials, such as hydroxychloroquine, chloroquine, or quinacrine, help relieve skin and joint symptoms and reduce the frequency of flare-ups.
People who have rashes or sores should stay out of direct sunlight and use strong sunscreens (with a sun protection factor of at least 50) when outside. Rashes may also be treated with corticosteroid creams or ointments or with an ointment that contains a medication called tacrolimus. (with a sun protection factor of at least 50) when outside. Rashes may also be treated with corticosteroid creams or ointments or with an ointment that contains a medication called tacrolimus.
If skin symptoms are not relieved by corticosteroid creams or ointments and hydroxychloroquine, people are given a combination of hydroxychloroquine and quinacrine or a combination of hydroxychloroquine and dapsone, methotrexate, mycophenolate mofetil, or azathioprine. If skin symptoms are not relieved by corticosteroid creams or ointments and hydroxychloroquine, people are given a combination of hydroxychloroquine and quinacrine or a combination of hydroxychloroquine and dapsone, methotrexate, mycophenolate mofetil, or azathioprine.
People whose symptoms are not controlled with other medications or who have frequent flare-ups may also be given belimumab, a medication that reduces the activity of certain white blood cells involved in the autoimmune response in people with lupus. Doctors periodically screen people for depression because this medication can start or worsen depression or thoughts and ideas about and preoccupation with death, particularly by suicide.People whose symptoms are not controlled with other medications or who have frequent flare-ups may also be given belimumab, a medication that reduces the activity of certain white blood cells involved in the autoimmune response in people with lupus. Doctors periodically screen people for depression because this medication can start or worsen depression or thoughts and ideas about and preoccupation with death, particularly by suicide.
Severe lupus
People who have severe, active lupus affecting the kidneys, heart, or brain, or causing lung bleeding are treated immediately, usually with the corticosteroid methylprednisolone given by vein (see People who have severe, active lupus affecting the kidneys, heart, or brain, or causing lung bleeding are treated immediately, usually with the corticosteroid methylprednisolone given by vein (seeCorticosteroids: Uses and Side Effects). Then people are given the corticosteroid prednisone taken by mouth. The dose and duration of treatment depend on which organs are affected. The immunosuppressant cyclophosphamide is also given to suppress the body’s autoimmune attack. Mycophenolate mofetil is a commonly used alternative for severe lupus affecting the kidneys because it is as effective as and less toxic than cyclophosphamide. Other immunosuppressants such as belimumab, voclosporin, or anifrolumab also help reduce lupus symptoms in some people.). Then people are given the corticosteroid prednisone taken by mouth. The dose and duration of treatment depend on which organs are affected. The immunosuppressant cyclophosphamide is also given to suppress the body’s autoimmune attack. Mycophenolate mofetil is a commonly used alternative for severe lupus affecting the kidneys because it is as effective as and less toxic than cyclophosphamide. Other immunosuppressants such as belimumab, voclosporin, or anifrolumab also help reduce lupus symptoms in some people.
People who have end-stage kidney disease can undergo a kidney transplantation as an alternative to dialysis.
People who have certain blood problems are given moderate or high doses of corticosteroids by mouth along with an immunosuppressant such as azathioprine or mycophenolate mofetil. They may be given immune globulin (a substance that contains large quantities of many antibodies) by vein. People who are not helped by those treatments may be given the immunosuppressant rituximab.People who have certain blood problems are given moderate or high doses of corticosteroids by mouth along with an immunosuppressant such as azathioprine or mycophenolate mofetil. They may be given immune globulin (a substance that contains large quantities of many antibodies) by vein. People who are not helped by those treatments may be given the immunosuppressant rituximab.
People who have nervous system problems may be given cyclophosphamide or rituximab by vein.People who have nervous system problems may be given cyclophosphamide or rituximab by vein.
People who develop blood clots are given heparin, warfarin, or other anticoagulants (medications that are sometimes called blood thinners). People who develop blood clots are given heparin, warfarin, or other anticoagulants (medications that are sometimes called blood thinners).
People with severe lupus often notice their symptoms have lessened after 4 to 12 weeks of treatment.
Maintenance medications
Once the initial inflammation is controlled, a doctor determines the lowest dose of corticosteroids and other medications that control inflammation (such as antimalarials and immunosuppressants) that is needed to most effectively suppress inflammation over the long term. Usually, the dose of prednisone is gradually decreased when symptoms are controlled and laboratory test results show improvement. Relapses or flare-ups can occur during this process. For most people who have lupus, the dose of prednisone can eventually be decreased or discontinued. Because the long-term use of high doses of corticosteroids leads to many side effects, people who need to take high doses of corticosteroids for a long time also are given an alternative medication to control inflammation such as azathioprine, methotrexate, or mycophenolate mofetil. Once the initial inflammation is controlled, a doctor determines the lowest dose of corticosteroids and other medications that control inflammation (such as antimalarials and immunosuppressants) that is needed to most effectively suppress inflammation over the long term. Usually, the dose of prednisone is gradually decreased when symptoms are controlled and laboratory test results show improvement. Relapses or flare-ups can occur during this process. For most people who have lupus, the dose of prednisone can eventually be decreased or discontinued. Because the long-term use of high doses of corticosteroids leads to many side effects, people who need to take high doses of corticosteroids for a long time also are given an alternative medication to control inflammation such as azathioprine, methotrexate, or mycophenolate mofetil.
People who take corticosteroids should be tested periodically and, if necessary, treated for osteoporosis, which can occur with chronic corticosteroid use. People who take high doses of corticosteroids for long periods are given supplements of calcium and vitamin Dsupplements of calcium and vitamin D and sometimes, for prevention, are given medications used to treat osteoporosis even if their bone density is normal.
People who are receiving immunosuppressants are also given medications to prevent infections such as by the fungus Pneumocystis jirovecii (see prevention of pneumonia in people with a weakened immune system) and vaccines against common infections such as pneumonia, influenza, and COVID-19.
Other medical conditions and pregnancy
All people should be monitored closely by a doctor for heart disease. Common risk factors for coronary artery disease (for example, high blood pressure, diabetes, and high cholesterol levels) should be controlled as well as possible.
Surgical procedures and pregnancy may be more complicated for people who have lupus, and they require close medical supervision. If pregnant, women should remain on hydroxychloroquine throughout their pregnancy and may be given low-dose aspirin as well. Pregnant women who are at risk of blood clots may be given heparin. Miscarriages and flare-ups during pregnancy are common. Surgical procedures and pregnancy may be more complicated for people who have lupus, and they require close medical supervision. If pregnant, women should remain on hydroxychloroquine throughout their pregnancy and may be given low-dose aspirin as well. Pregnant women who are at risk of blood clots may be given heparin. Miscarriages and flare-ups during pregnancy are common.
Women should avoid becoming pregnant during a flare-up. Because mycophenolate mofetil causes birth defects, women should wait to become pregnant until their disease has been well controlled for 6 months or longer (see Women should avoid becoming pregnant during a flare-up. Because mycophenolate mofetil causes birth defects, women should wait to become pregnant until their disease has been well controlled for 6 months or longer (seelupus during pregnancy). Women who are in remission and who are thinking about becoming pregnant but who need to keep taking maintenance medications are usually switched from mycophenolate mofetil to azathioprine at least 6 months before conceiving.). Women who are in remission and who are thinking about becoming pregnant but who need to keep taking maintenance medications are usually switched from mycophenolate mofetil to azathioprine at least 6 months before conceiving.
Prognosis for Lupus
Lupus tends to be chronic and relapsing, often with symptom-free periods (remissions) that can last for years. Flare-ups in women occur less often after menopause.
Many people are being diagnosed earlier and with milder lupus than in the past, and better treatment is available. As a result, in countries where people have access to good health care, almost 90% of people live for at least 10 years after the diagnosis is made. However, because the course of lupus is unpredictable, the prognosis varies widely. Usually, if the first bout of inflammation is controlled, the long-term prognosis is good. However, despite better treatment and a lower death rate, people who have lupus may not live as long as people who do not because of they have an increased risk of heart disease, end-stage kidney disease, and infection.
More Information
The following English-language resource may be useful. Please note that The Manual is not responsible for the content of this resource.
Lupus Foundation of America: Provides information about living with lupus and ongoing lupus research