Diverticulitis is inflammation with or without infection of a diverticulum, which can result in phlegmon of the bowel wall, peritonitis, perforation, fistula, or abscess. The primary symptom is abdominal pain. Diagnosis is by CT and ultrasound. Treatment is with bowel rest, sometimes antibiotics, and occasionally surgery.
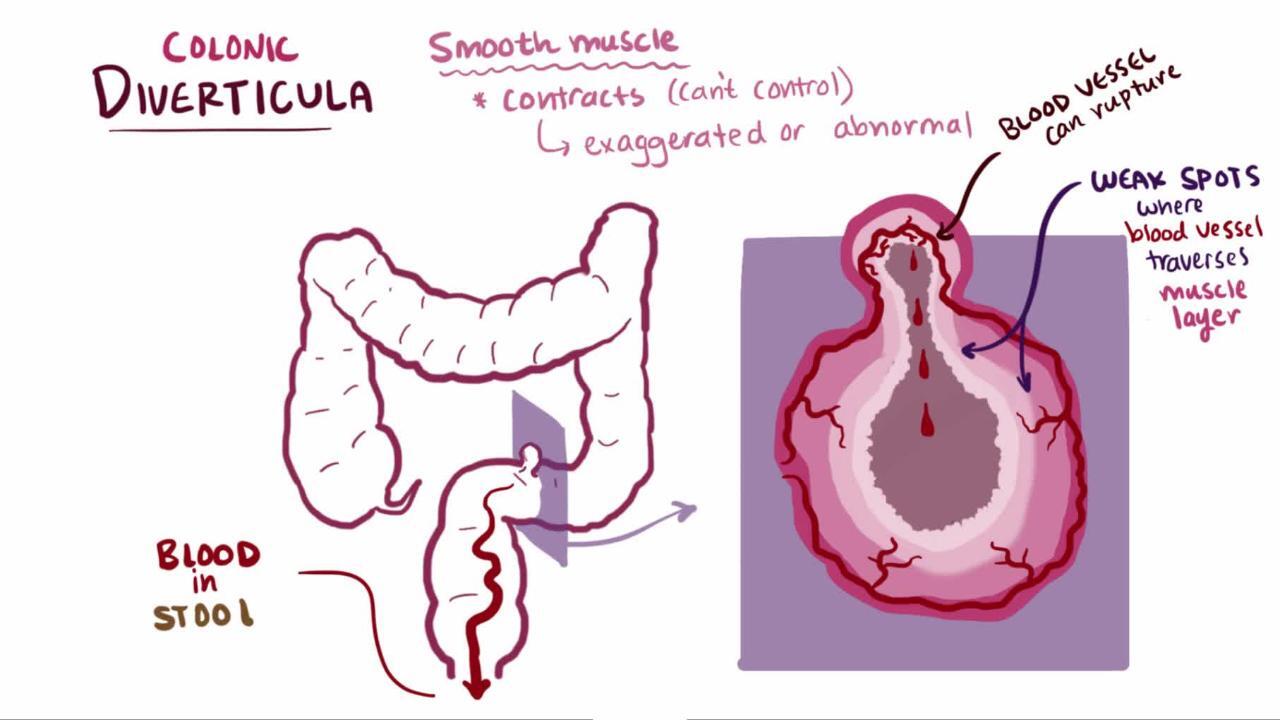
A colonic diverticulum is a saclike pouch of colonic mucosa and submucosa that protrudes through the muscular layer of the colon; because it does not contain all layers of the bowel, it is considered a pseudodiverticulum (see also Definition of Diverticular Disease).
Many people have multiple colonic diverticula (diverticulosis). In people > 50 years, acute diverticulitis is most common among women; in those < 50 years, it is most common among men. Distal diverticulitis is more common among White people (1).
Patients with HIV infection and those undergoing chemotherapy are at increased risk of developing acute diverticulitis (2).
Diverticula are usually asymptomatic but sometimes become inflamed (diverticulitis). One study reported that 4.3% of patients with documented diverticulosis developed diverticulitis over an 11-year follow-up period (3).
Diverticulitis that is managed nonoperatively can recur as either an acute or chronic process. The risk of a recurrent acute episode is up to 39%, although reported rates vary widely (4). A large population-based study found that after an episode of acute diverticulitis the recurrence rate at 1 year was 8% and at 10 years was 22% (5). In some patients, however, recurrence manifests as chronic, ongoing abdominal pain; this may develop after 1 or more acute episodes.
General references
1. Gunby SA, Strate LL. Acute Colonic Diverticulitis. Ann Intern Med. 2024;177(3):ITC33-ITC48. doi:10.7326/AITC202403190
2. Francis NK, Sylla P, Abou-Khalil M, et al. EAES and SAGES 2018 consensus conference on acute diverticulitis management: Evidence-based recommendations for clinical practice. Surg Endosc. 2019;33(9):2726–2741. doi:10.1007/s00464-019-06882-z
3. Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11(12):1609–1613. doi:10.1016/j.cgh.2013.06.020
4. Sallinen V, Mali J, Leppäniemi A, Mentula P. Assessment of risk for recurrent diverticulitis: A proposal of risk score for complicated recurrence. Medicine (Baltimore). 2015;94(8):e557. doi:10.1097/MD.0000000000000557
5. Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal trends in the incidence and natural history of diverticulitis: A population-based study. Am J Gastroenterol. 2015;110(11):1589–1596. doi:10.1038/ajg.2015.302
Etiology of Colonic Diverticulitis
The etiology and pathophysiology of diverticulitis are not fully understood and may vary among patients. It has long been thought that diverticulitis occurs when a micro or macro perforation develops in a diverticulum, resulting in the release of intestinal bacteria and triggering inflammation. However, emerging data suggest that in some patients, acute diverticulitis is more of an inflammatory than infectious process. Furthermore, cytomegalovirus may be a trigger of that inflammation; active viral replication has been found in affected colon tissue in over two-thirds of patients with diverticulitis.
Studies have suggested a direct correlation between red meat consumption per week, smoking, obesity, and the incidence of diverticulitis (1, 2). Nonsteroidal anti-inflammatory drugs, aspirin, corticosteroids, and opioids also increase the risk of diverticulosis and diverticulitis (3, 4). There is no association between consumption of nuts, seeds, corn, or popcorn and development of diverticulitis as was previously thought.
Physical activity and dietary fiber have been shown to help prevent formation of diverticula and development of diverticulitis (3, 4).
Etiology references
1. Cao Y, Strate LL, Keeley BR, et al: Meat intake and risk of diverticulitis among men. Gut pii: gutjnl-2016-313082, 2017. doi: 10.1136/gutjnl-2016-313082
2. Strate LL, Keeley BR, Cao Y, et al: Western dietary pattern increases, and prudent dietary pattern decreases, risk of incident diverticulitis in a prospective cohort study. Gastroenterology 152(5):1023–1030.e2, 2017. doi: 10.1053/j.gastro.2016.12.038
3. Bohm SK, Kruis W: Lifestyle and other risk factors for diverticulitis. Minerva Gastroenterol Dietol 63(2):110–118, 2017. doi: 10.23736/S1121-421X.17.02371-6
4. Schultz JK, Azhar N, Binda GA, et al: European Society of Coloproctology: Guidelines for the management of diverticular disease of the colon. Colorectal Dis 22 (supplement 2):S5–S28, 2020. doi: 10.1111/codi.15140
Classification of Colonic Diverticulitis
Acute diverticulitis can be classified as
Acute uncomplicated diverticulitis: This is the most common manifestation of acute diverticulitis.
Acute complicated diverticulitis: This manifestation is defined by the presence of abscess, fistula, obstruction, or free perforation; 2 classifications exist (eg, see table Classification of Acute Complicated Diverticulitis). Approximately 12% of patients with diverticulitis present with complicated disease (1).
Complications can develop after perforation of an inflamed diverticulum.
Approximately 15% of patients with acute complicated diverticulitis have a pericolic or intramesenteric abscess (2).
If acute diverticulitis does not heal completely, chronic diverticulitis will develop.
Chronic diverticulitis can be classified as
Chronic uncomplicated diverticulitis: Defined as thickening of the colonic wall or chronic mucosal inflammation in the absence of stricture
Chronic complicated diverticulitis: Includes stenotic disease, which may cause acute colon obstruction and fistula formation (most commonly to the bladder)
Classification references
1. Gunby SA, Strate LL. Acute Colonic Diverticulitis. Ann Intern Med. 2024;177(3):ITC33-ITC48. doi:10.7326/AITC202403190
2. Lambrichts DPV, Bolkenstein HE, van der Does DCHE, et al: Multicentre study of non-surgical management of diverticulitis with abscess formation. Br J Surg. 2019;106(4):458-466. doi:10.1002/bjs.11129
Symptoms and Signs of Colonic Diverticulitis
Patients have left lower quadrant abdominal pain and tenderness and often have a palpable sigmoid; pain is occasionally suprapubic. However, Asian patients with diverticulitis often present with right-sided pain due to right colon involvement. The pain can be accompanied by nausea, vomiting, fever, and sometimes even urinary symptoms as a result of bladder irritation.
Peritoneal signs (eg, rebound or guarding) may be present, particularly with abscess or free perforation.
Fistula may manifest as pneumaturia, fecaluria (feces in the urine), feculent vaginal discharge, or a cutaneous or myofascial infection of the abdominal wall, perineum, or upper leg. Patients with bowel obstruction have nausea, vomiting, and abdominal distention. Bleeding is uncommon.
Recurrent episodes of acute diverticulitis manifest similarly to initial episodes; they are not necessarily more severe.
Photo courtesy of Drs. Joel A. Baum and Rafael A. Ching Companioni.
Diagnosis of Colonic Diverticulitis
Abdominal and pelvic CT
Point-of-care ultrasound
Colonoscopy after resolution
Clinical suspicion is high in patients with known diverticulosis who present with characteristic abdominal symptoms. However, because other disorders (eg, appendicitis, colon or ovarian cancer, inflammatory bowel disease) may cause similar symptoms, testing is required.
LIVING ART ENTERPRISES, LLC/SCIENCE PHOTO LIBRARY
Diverticulitis is evaluated with CT of the abdomen and pelvis with water-soluble contrast given orally and rectally; IV contrast also is given when not contraindicated. However, findings in approximately 10% of patients cannot distinguish diverticulitis from colon cancer. MRI is an alternative for pregnant and young patients (1, 2).
Point-of-care ultrasound in an emergency department or urgent care facility could be an option for people with diverticulitis. Although ultrasound has been shown to have a high sensitivity (95%) and specificity (76%) for the diagnosis of diverticulitis compared with CT, it is less sensitive (55%) in distinguishing complicated from simple diverticulitis (3).
Colonoscopy is often recommended 1 to 3 months after resolution of the episode to assess for cancer. However, in the absence of high-risk signs (eg, complicated diverticulitis, uncomplicated diverticulitis with imaging abnormalities or atypical course, family history of colorectal cancer, anemia, weight loss), the likelihood of malignant lesions or advanced adenomas after an episode of acute uncomplicated diverticulitis is low (2).
Diagnosis references
1. Stewart DB. Review of the American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. JAMA Surg. 2021;156(1):94–95. doi:10.1001/jamasurg.2020.5019
2. Francis NK, Sylla P, Abou-Khalil M, et al. EAES and SAGES 2018 consensus conference on acute diverticulitis management: Evidence-based recommendations for clinical practice. Surg Endosc. 2019;33(9):2726–2741. doi:10.1007/s00464-019-06882-z
3. Shokoohi H, Selame LA, Loesche MA, et al. Accuracy of "TICS" ultrasound protocol in detecting simple and complicated diverticulitis: A prospective cohort study. Acad Emerg Med. 2023;30(3):172-179. doi:10.1111/acem.14628
Treatment of Colonic Diverticulitis
Varies with severity
Sometimes antibiotics
CT-guided percutaneous drainage of abscess
Sometimes surgery
A patient who is not very ill is treated at home with rest. Symptoms usually subside rapidly.
For patients with uncomplicated diverticulitis, a clear liquid diet for 2 to 3 days is recommended with advancement to a low-fiber diet when pain abates (1).
Patients with more severe symptoms (eg, moderate to severe pain, fever, marked leukocytosis) should be hospitalized, as should patients taking prednisone (who are at higher risk of perforation and general peritonitis). Treatment is bed rest, nothing by mouth (for patients with acute complicated diverticulitis), and IV fluids.Patients with more severe symptoms (eg, moderate to severe pain, fever, marked leukocytosis) should be hospitalized, as should patients taking prednisone (who are at higher risk of perforation and general peritonitis). Treatment is bed rest, nothing by mouth (for patients with acute complicated diverticulitis), and IV fluids.
Antibiotics
Antibiotics were traditionally recommended for all cases of acute diverticulitis whether or not they were complicated. However, data suggest that antibiotics may not improve outcome in uncomplicated diverticulitis; therefore, patients who are otherwise healthy and have uncomplicated sigmoid diverticulitis can sometimes be safely managed without antibiotics; antibiotic therapy should be considered on a case-by-case basis (1, 2).
Antibiotic therapy should be used for patients with acute complicated diverticulitis, immunosuppression, sepsis, or significant comorbidities.
If antibiotics are used, they should cover gram-negative bacilli and anaerobic bacteria.
Oral antibiotic regimens that can be given to outpatients for whom treatment is elected include 7 to 10 days of one of the following:
Metronidazole plus a fluoroquinolone (eg, ciprofloxacin)Metronidazole plus a fluoroquinolone (eg, ciprofloxacin)
Metronidazole plus a cephalosporin (eg, cephalexin)Metronidazole plus a cephalosporin (eg, cephalexin)
Metronidazole plus trimethoprim/sulfamethoxazole Metronidazole plus trimethoprim/sulfamethoxazole
Amoxicillin plus clavulanic acidAmoxicillin plus clavulanic acid
Moxifloxacin (for patients unable to take penicillins or metronidazole)Moxifloxacin (for patients unable to take penicillins or metronidazole)
IV antibiotic regimens for hospitalized patients are selected based on many factors, including the severity of illness, risk of adverse outcome (eg, due to other illnesses, older age, immunosuppression), and likelihood of resistant organisms. Many regimens exist, such as a combination of metronidazole plus a cephalosporin or a fluoroquinolone. Single-antibiotic regimens include ertapenem, moxifloxacin, ticarcillin/clavulanic acid, imipenem/cilastatin, meropenem, doripenem, and piperacillin/tazobactam.IV antibiotic regimens for hospitalized patients are selected based on many factors, including the severity of illness, risk of adverse outcome (eg, due to other illnesses, older age, immunosuppression), and likelihood of resistant organisms. Many regimens exist, such as a combination of metronidazole plus a cephalosporin or a fluoroquinolone. Single-antibiotic regimens include ertapenem, moxifloxacin, ticarcillin/clavulanic acid, imipenem/cilastatin, meropenem, doripenem, and piperacillin/tazobactam.
There are no well-defined standards relating abscess size to the need for surgery or interventional (ultrasound- or CT-guided) drainage. However, small pericolic abscesses (less than 2 to 3 cm in diameter) often resolve with broad-spectrum antibiotics and bowel rest alone.
If response is satisfactory, the patient remains hospitalized until symptoms are relieved; a soft diet is resumed as tolerated. After the episode resolves, patients should consume a high-fiber diet and avoid routine analgesic use of nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin to prevent recurrence.
Percutaneous drainage or endoscopic ultrasound-guided drainage
CT-guided percutaneous or endoscopic ultrasound-guided drainage is becoming the standard of care for larger abscesses (over 3 cm in diameter), for abscesses that do not resolve with antibiotics, and/or for clinical deterioration. However, abscesses that are multiloculated, inaccessible, or not improving with drainage require surgical intervention.
Surgery
Surgery is required immediately for patients with free perforation or when feculent peritonitis is suspected based on clinical examination or imaging. Other indications for surgery include severe symptoms that do not respond to nonsurgical treatment within 3 to 5 days and increasing pain, tenderness, and fever. Approximately 15 to 20% of people admitted with acute diverticulitis require surgery during that admission (3).
For uncomplicated diverticulitis, surgical resection was previously recommended based on the number of recurrences. Currently, the American Society of Colon and Rectal Surgeons (ASCRS) and other practice guidelines recommend a case-by-case evaluation rather than mandatory elective segmental colectomy after a second episode (4–8; see also the Japan Gastroenterological Association's 2019 guidelines for colonic diverticular bleeding and colonic diverticulitis). Patients for whom recurrent attacks pose a higher risk of death or complications are typically considered candidates for surgery.
For complicated diverticulitis, surgical recommendations vary. An elective segmental colectomy is not routinely recommended for patients after a conservatively managed episode of acute complicated diverticulitis (9). Surgery is recommended for patients with chronic complicated diverticulitis where fistulas and persisting abscesses are present.
The involved section of the colon is resected. The ends can be reanastomosed immediately in healthy patients without perforation, abscess, or significant inflammation. Other patients have a temporary colostomy with anastomosis carried out in a subsequent operation after inflammation resolves and their general condition improves.
Treatment references
1. Gunby SA, Strate LL. Acute Colonic Diverticulitis. Ann Intern Med. 2024;177(3):ITC33-ITC48. doi:10.7326/AITC202403190
2. Peery AF, Shaukat A, Strate LL. AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review. Gastroenterology. 2021;160(3):906-911.e1. doi:10.1053/j.gastro.2020.09.059
3. Wieghard N, Geltzeiler CB, Tsikitis VL. Trends in the surgical management of diverticulitis. Ann Gastroenterol. 2015;28(1):25–30.
4. Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–294. doi:10.1097/DCR.0000000000000075
5. Regenbogen SE, Hardiman KM, Hendren S, Morris AM. Surgery for diverticulitis in the 21st century: A systematic review. JAMA Surg. 2014;149(3):292–303. doi:10.1001/jamasurg.2013.5477
6. Comparato G, Di Mario F. Recurrent diverticulitis. J Clin Gastroenterol. 2008;42(10):1130–1134. doi:10.1097/MCG.0b013e3181886ee4
7. Young-Fadok TM. Diverticulitis. N Engl J Med. 2018;379(17):1635–1642. doi:10.1056/NEJMcp1800468
8. Hall J, Hardiman K, Lee S, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis Colon Rectum. 2020;63(6):728-747. doi:10.1097/DCR.0000000000001679
9. Schultz JK, Azhar N, Binda GA, et al. European Society of Coloproctology: Guidelines for the management of diverticular disease of the colon. Colorectal Dis. 2020;22(supplement 2):S5–S28. doi:10.1111/codi.15140
Key Points
Diverticulitis is inflammation and/or infection of a diverticulum.
Inflammation remains uncomplicated in most patients; the remainder develop abscesses, peritonitis, bowel obstruction, or fistulas.
Diagnose using abdominal and pelvic CT with oral, rectal, and IV contrast; do colonoscopy 1 to 3 months after the episode to look for cancer.
Management depends on severity but typically includes conservative management, often antibiotics, and sometimes percutaneous or endoscopic ultrasound-guided drainage or surgical resection.
More Information
The following English-language resources may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
Japan Gastroenterological Association: Guidelines for colonic diverticular bleeding and colonic diverticulitis (2019)
American Society of Colon and Rectal Surgeons: Guidelines for the treatment of left-sided colonic diverticulitis (2020)
Segmental Colitis Associated With Diverticulosis (SCAD)
(See also Colonic Diverticulosis.)
Segmental colitis associated with diverticulosis (SCAD) and chronic recurrent diverticulitis are terms used to describe chronic colonic inflammation attributed to diverticulosis. SCAD usually affects the interdiverticular mucosa and is usually present on the left side sparing the rectum and ascending colon.
The cause of SCAD is unknown and may be multifactorial. Mucosal prolapse, fecal stasis, localized ischemia, alterations in the gut microbiota, and/or chronic inflammation may play a role. It is unclear how much the relationship between the diverticulosis and colitis is causal, is due to a common underlying factor, or is coincidental: the histologic characteristics contain features similar to those seen in inflammatory bowel disease, infectious colitis, and ischemic colitis. The prevalence of SCAD in people with diverticulosis is very low (1%). SCAD usually affects males > 60 years of age (1).
Reference
1. Sbarigia C, Ritieni C, Annibale B, Carabotti M. Common Diagnostic Challenges and Pitfalls in Segmental Colitis Associated with Diverticulosis (SCAD). J Clin Med. 2023;12(18):6084. Published 2023 Sep 20. doi:10.3390/jcm12186084
Symptoms and Signs
Symptoms of SCAD include hematochezia, lower abdominal pain, change in bowel habits, and diarrhea.
Fever, nausea, vomiting, and weight loss are infrequent symptoms.
Diagnosis
Endoscopy
The diagnosis of SCAD is suggested when endoscopy reveals erythematous, friable, and granular mucosa with either a diffuse or patchy distribution involving the interdiverticular mucosa.
Treatment
Symptom relief
Treatment of SCAD is symptomatic; to date, high-quality randomized clinical trials have not been done.
Initial treatment with the oral antibiotics ciprofloxacin and metronidazole is recommended. In patients who do not improve with antibiotics, oral preparations of 5-aminosalicylic acid (5-ASA) can be used. Corticosteroids (eg, prednisone) are used for refractory cases. Initial treatment with the oral antibiotics ciprofloxacin and metronidazole is recommended. In patients who do not improve with antibiotics, oral preparations of 5-aminosalicylic acid (5-ASA) can be used. Corticosteroids (eg, prednisone) are used for refractory cases.
Surgery (segmental colectomy) is an option for patients with corticosteroid-refractory or corticosteroid-dependent SCAD.