Dilated cardiomyopathy is a group of heart muscle disorders in which the ventricles (the 2 lower chambers of the heart) enlarge (dilate) but are not able to pump enough blood for the body’s needs, resulting in heart failure.
Topic Resources
Viral infections, genetic disorders, and some hormonal disorders are common causes of dilated cardiomyopathy, but often the cause is unknown.
Shortness of breath and fatigue are often the first symptoms.
Electrocardiography (ECG), echocardiography, and magnetic resonance imaging (MRI) are used to diagnose dilated cardiomyopathy.
Doctors try to treat the cause of this cardiomyopathy, usually by giving medications.
Cardiomyopathy refers to progressive impairment of the structure and function of the muscular walls of the heart chambers. There are 3 main types of cardiomyopathy. In addition to dilated cardiomyopathy, there are hypertrophic cardiomyopathy and restrictive cardiomyopathy (see also Overview of Cardiomyopathy).
The term cardiomyopathy is used only when a disorder directly affects the heart muscle. Other heart disorders, such as coronary artery disease and heart valve disorders, also can eventually cause the ventricles to enlarge, leading to heart failure.
Dilated cardiomyopathy can develop at any age but is more common in adults younger than about 50 years of age. About 10% of people who develop dilated cardiomyopathy are older than 65. In the United States, the disorder occurs more often in males than in females as well as more often in people with African ancestry compared with White people. About 7 of every 100,000 people develop dilated cardiomyopathy each year.
Causes of Dilated Cardiomyopathy
The most common causes of dilated cardiomyopathy are
Viral infections
Genetic disorders (genetic factors play a role in 20 to 35% of cases)
Some viral infections can cause an acute inflammation of the heart muscle (myocarditis). When inflammation damages the heart's pumping ability, the disorder is called viral cardiomyopathy. In North America, infection with coxsackie B virus is the most common cause of viral cardiomyopathy. HIV infection also can cause cardiomyopathy. In other parts of the world, other viral infections are more common causes. Occasionally, dilated cardiomyopathy results from a bacterial infection, such as Chagas disease.
The virus or bacteria infects and often weakens the heart muscle. As a result, the heart cannot pump as forcefully. The damaged heart muscle is replaced by fibrous (scar) tissue. The heart muscle then stretches resulting in enlargement of the heart chambers and reduced pumping ability. After that point, heart failure develops.
Other causes of dilated cardiomyopathy include
Certain chronic hormonal disorders such as long-standing, poorly controlled diabetes mellitus or poorly controlled thyroid disease
Severe obesity
Rapid heart rate (persistent)
Use of alcohol (when intake is heavy and undernutrition is also present), cocaine, some antidepressants, some antipsychotic medications, and a few chemotherapy agents
In many cases, a definite cause of dilated cardiomyopathy cannot be identified in which case it is called idiopathic dilated cardiomyopathy.
Rare causes of dilated cardiomyopathy include pregnancy (peripartum cardiomyopathy), iron overload, sarcoidosis, and systemic rheumatic disorders such as rheumatoid arthritis, systemic lupus erythematosus (lupus), and systemic sclerosis. Extreme stress can also sometimes cause a type of dilated cardiomyopathy called Takotsubo cardiomyopathy, stress cardiomyopathy, or broken heart syndrome.
Symptoms of Dilated Cardiomyopathy
Usually, the first symptoms of dilated cardiomyopathy are becoming short of breath during exertion and tiring easily. These symptoms result from a weakening of the heart’s pumping action, which is called heart failure. Some people have chest pain.
When cardiomyopathy results from an infection, the first symptoms may be a sudden fever and flu-like symptoms.
Complications
Heart failure can develop when heart damage is severe no matter the cause of dilated cardiomyopathy. If heart failure occurs, fluid is retained in the legs and abdomen (causing swelling), and the lungs fill with fluid (causing shortness of breath with physical activity and while lying flat). When heart failure is severe, blood pressure can be low due to the weakness of the heart.
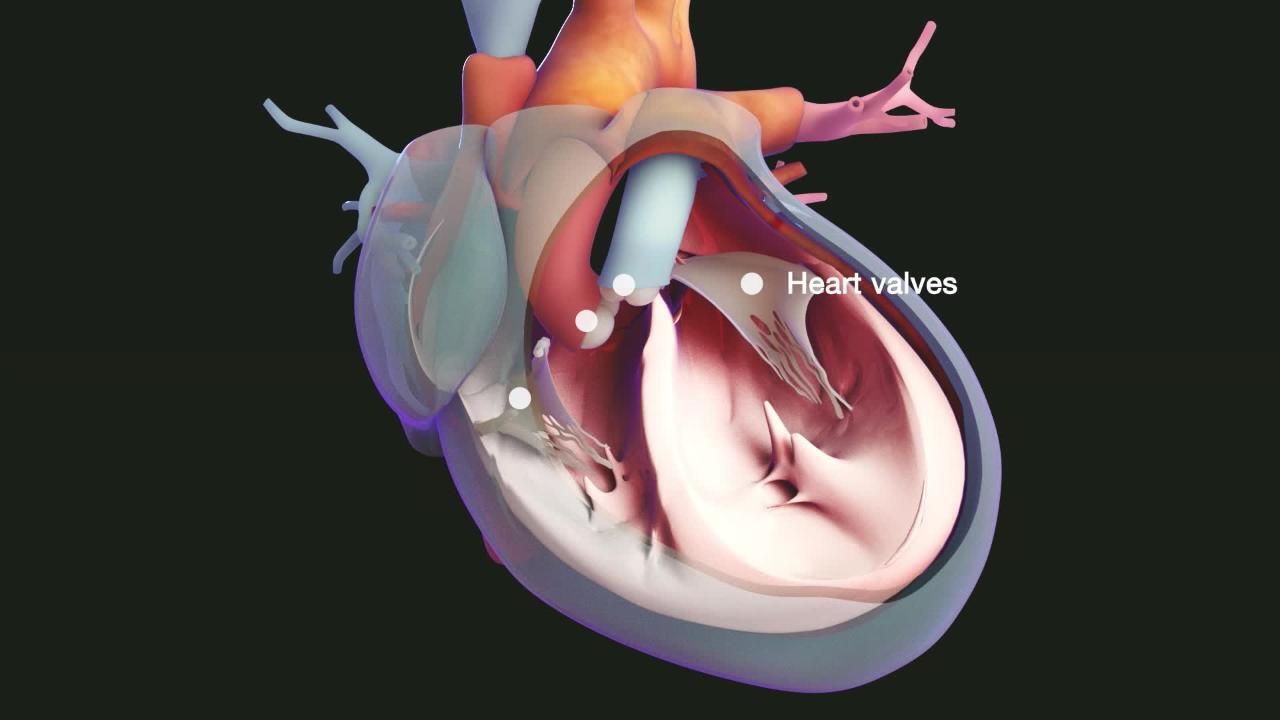
Heart valve problems may develop. Because the heart is enlarged, the heart valves may be unable to close normally and often allow blood to leak back into the heart chamber rather than flowing into the next blood vessel or chamber (called regurgitation). The valves most often affected are the mitral valve, which is positioned between the left atrium (upper heart chamber) and the left ventricle (lower heart chamber), and the tricuspid valve, which is positioned between the right atrium and the right ventricle. Leakage causes heart murmurs, which doctors can hear with a stethoscope.
Abnormal heart rhythms (arrhythmias) can result from damage to and stretching of the heart muscle. Arrhythmias may cause sensation of irregular heartbeats (palpitations), shortness of breath, or sudden death. The leakage of the valves and the abnormal heart rhythms may interfere further with the heart’s pumping action.
Blood clots may form on heart chamber walls because blood can pool in the enlarged heart, particularly when the ventricles are very dilated and poorly contracting. The clots can break into pieces (becoming emboli), travel from the heart to blood vessels elsewhere in the body, and block them, causing damage to the organ they supply. If the blood supply to the brain is blocked, a stroke can result.
Diagnosis of Dilated Cardiomyopathy
Imaging tests such as echocardiography or magnetic resonance imaging (MRI) of the heart
Sometimes, a biopsy of the heart muscle
Sometimes, testing for the cause and/or complications
The diagnosis of dilated cardiomyopathy is based on the person's symptoms, the results of a physical examination, and additional tests. Doctors look for other causes of a dilated heart, such as a previous heart attack, chronic high blood pressure, or a damaged heart valve.
Blood tests for common viruses that can cause dilated cardiomyopathy are done when doctors suspect infection as a cause.
Electrocardiography (ECG) may detect abnormalities in the electrical activity of the heart. However, these abnormalities are usually not sufficient evidence for a diagnosis.
Because genetic disorders may cause dilated cardiomyopathy, family members may also be tested.
Imaging of the heart
Echocardiography, which uses ultrasound waves to produce an image of the heart, is the most useful procedure because it can show both the size and pumping action of the heart.
Cardiac magnetic resonance imaging (MRI), which produces very detailed images of the heart, is more often being used to confirm the diagnosis (and sometimes identify the cause).
Biopsy and cardiac catheterization
If the diagnosis remains in doubt, cardiac catheterization, an invasive procedure in which a catheter is threaded from a blood vessel in the arm, neck, or leg into the heart, can provide additional information about the pumping ability of the heart. During cardiac catheterization, doctors can also obtain a biopsy (remove a tissue sample from inside the heart for examination under a microscope), measure pressures in the heart chambers, and exclude coronary artery disease.
Treatment of Dilated Cardiomyopathy
Medications
Sometimes, device therapy with a defibrillator and/or pacemaker
If possible, doctors treat the disorder that is causing the dilated cardiomyopathy. For example, medications that suppress the immune system (immunosuppressants) such as corticosteroids may be used to treat a systemic rheumatic disorder that caused dilated cardiomyopathy.
General treatment measures include avoiding stress, limiting salt in the diet, and having periods of rest, which help reduce strain on the heart, particularly when the cardiomyopathy is acute or severe.
Medications for dilated cardiomyopathy
Medications used for heart failure, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, a combination angiotensin II receptor blocker and neprilysin inhibitor, aldosterone antagonists (spironolactone or eplerenone), sodium glucose cotransporter 2 protein (SGLT) inhibitors, the combination of hydralazine and nitrates, and ivabradine, improve the heart’s pumping function, prolong life, and help to decrease persistent symptoms. antagonists (spironolactone or eplerenone), sodium glucose cotransporter 2 protein (SGLT) inhibitors, the combination of hydralazine and nitrates, and ivabradine, improve the heart’s pumping function, prolong life, and help to decrease persistent symptoms.
Diuretics (medications that increase urination) are used to reduce excess fluid in the lungs and decrease symptoms of swelling due to fluid retention, but they do not prolong life.
Digoxin may help the heart's pumping and decrease the number of hospitalizations for heart failure, but it does not prolong life.Digoxin may help the heart's pumping and decrease the number of hospitalizations for heart failure, but it does not prolong life.
Antiarrhythmic medications may be given to treat abnormal heart rhythms. Most of these medications are initially prescribed in low doses. Doses are increased in small increments because if the dose is too large, an antiarrhythmic medication may worsen heart rhythm abnormalities or depress pumping function.
Medications to prevent blood clots, such as warfarin or aspirin, may be used, particularly when ventricles are very dilated and contracting poorly.Medications to prevent blood clots, such as warfarin or aspirin, may be used, particularly when ventricles are very dilated and contracting poorly.
Special precautions are needed when medications are given to women with peripartum cardiomyopathy because some of the medications usually used to treat cardiomyopathy may be absorbed into breast milk and harm nursing infants.
Device therapy
Some people have an abnormality of the electrical conduction in the heart, which can be helped by an artificial pacemaker that stimulates first the atria and then both ventricles (cardiac resynchronization therapy). This type of pacemaker, when used in the right person, will help to return the contraction pattern of the heart toward normal and improve its function.
Doctors may also consider an implantable cardioverter-defibrillator pacemaker in people who have persistently poor heart function and an increased risk of arrhythmias leading to sudden death.
Heart transplantation
Heart failure in dilated cardiomyopathy can be progressive and ultimately fatal. Because of this poor prognosis, dilated cardiomyopathy is the most common reason for heart transplantation or mechanical heart support with a left ventricular assist device. Successful heart transplantation cures the disorder, but it has its own complications and limitations.
Prognosis for Dilated Cardiomyopathy
The prognosis of dilated cardiomyopathy varies considerably depending on many factors. In general, the prognosis worsens as the heart becomes more dilated and functions less well. Abnormal heart rhythms also indicate a worse prognosis. Overall, the prognosis is better for females than males, and people with African ancestry survive half as long as White people.
About 40 to 50% of deaths are sudden, probably resulting from an abnormal heart rhythm or an blood clot that blocks blood flow in a critical area. Additional factors that influence the risk of death include the cause and severity of the cardiomyopathy, the person's age and ability to follow medical advice (including taking medications as directed, maintaining a low-salt diet, and attending scheduled follow-up health care appointments), and whether the person has access to specialized treatment. However, overall prognosis has improved with the introduction of implantable cardioverter-defibrillators, cardiac resynchronization therapy, and other interventions.
More Information
The following English-language resource may be useful. Please note that THE MANUAL is not responsible for the content of this resource.
American Heart Association: Dilated cardiomyopathy: Provides comprehensive information on symptoms, diagnosis, and treatment of dilated cardiomyopathy