Cerebral palsy refers to a group of nonprogressive conditions characterized by impaired voluntary movement or posture and resulting from prenatal developmental malformations or perinatal or postnatal central nervous system damage. Cerebral palsy manifests before age 2 years. Diagnosis is clinical. Treatment may include physical and occupational therapy, braces, medications or botulinum toxin injections, orthopedic surgery, intrathecal baclofen, or, in certain cases, dorsal rhizotomy.Cerebral palsy refers to a group of nonprogressive conditions characterized by impaired voluntary movement or posture and resulting from prenatal developmental malformations or perinatal or postnatal central nervous system damage. Cerebral palsy manifests before age 2 years. Diagnosis is clinical. Treatment may include physical and occupational therapy, braces, medications or botulinum toxin injections, orthopedic surgery, intrathecal baclofen, or, in certain cases, dorsal rhizotomy.
Topic Resources
Cerebral palsy (CP) is a group of conditions that causes nonprogressive spasticity, ataxia, or involuntary movements; it is not a specific disorder or single condition.
CP occurs in 2 to 3/1000 live births. The highest prevalence, 111.8/1000 live births, occurs in preterm infants < 28 weeks gestation (1).
Reference
1. Wimalasundera N, Stevenson VL: Cerebral palsy. Pract Neurol 16(3):184–194, 2016. doi: 10.1136/practneurol-2015-001184
Etiology of Cerebral Palsy
Etiology of cerebral palsy is multifactorial, and a specific cause is sometimes hard to establish. Prematurity, in utero disorders, neonatal encephalopathy, and kernicterus often contribute. Perinatal factors (eg, perinatal asphyxia, stroke, central nervous system [CNS] infections) probably cause 15 to 20% of cases.
Examples of types of CP are
Spastic diplegia after preterm birth
Spastic quadriparesis after perinatal asphyxia
Athetoid and dystonic forms after perinatal asphyxia or kernicterus
CNS trauma or a severe systemic disorder (eg, stroke, meningitis, sepsis, dehydration) during early childhood (before 2 years of age) may also cause CP.
Symptoms and Signs of Cerebral Palsy
Before a specific type develops, symptoms include lagging motor development and often persistent infantile reflex patterns, hyperreflexia, and altered muscle tone.
Types of cerebral palsy
CP is categorized mainly as one of the following, depending on which parts of the CNS are malformed or damaged (1, 2):
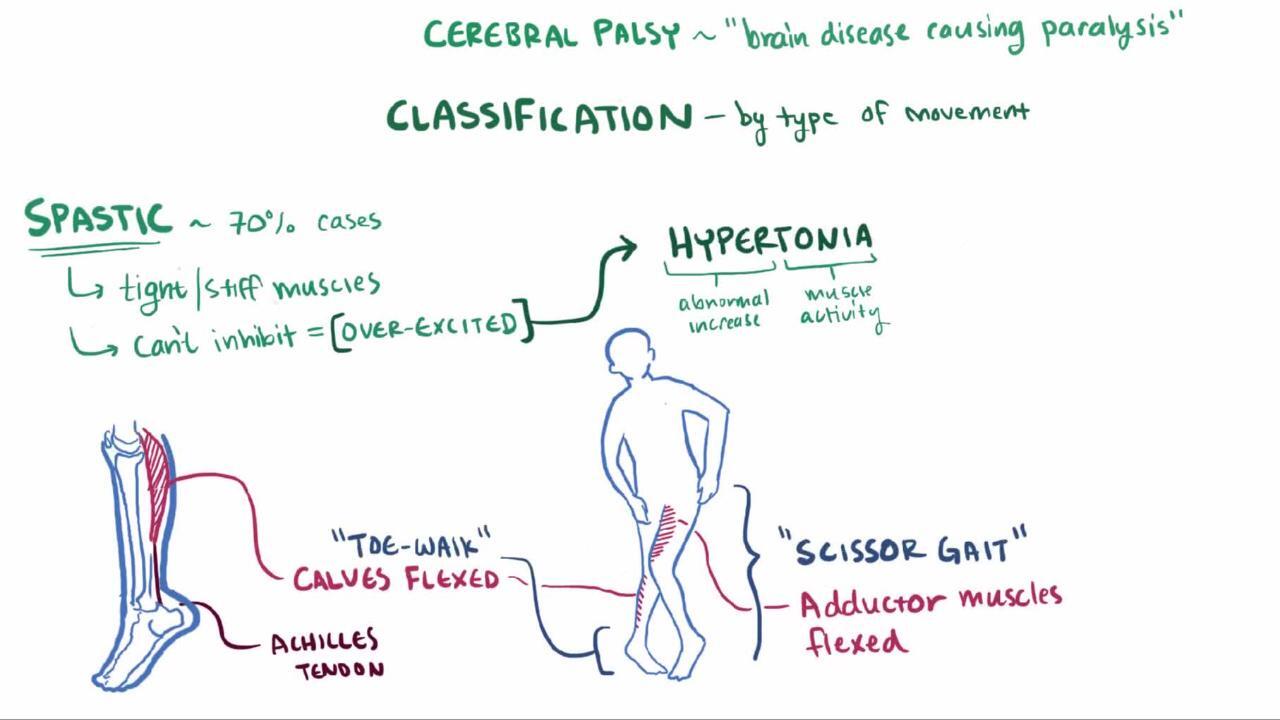
Spastic CP is the most common type and occurs in > 80% of cases (2). Spasticity is a state of resistance to passive range of motion; resistance increases with increasing speed of that motion. It is due to upper motor neuron involvement and may mildly or severely affect motor function. Spastic CP may cause hemiplegia, quadriplegia, diplegia, or paraplegia. Usually, deep tendon reflexes in affected limbs are increased, muscles are hypertonic, and voluntary movements are weak and poorly coordinated. Joint contractures develop, and joints may become misaligned. A scissors gait and toe walking are typical. In mild cases, impairment may occur only during certain activities (eg, running). Corticobulbar impairment of oral, lingual, and palatal movement, with consequent dysarthria or dysphagia, commonly occurs with quadriplegia.
Athetoid CP or dyskinetic CP is the second most common type. It occurs in about 15% of cases and results from basal ganglia involvement. Athetoid or dyskinetic CP is defined by slow, writhing, involuntary movements of the proximal extremities and trunk (athetoid movements), often activated by attempts at voluntary movement or by excitement. Abrupt, jerky, distal (choreic) movements may also occur. Movements increase with emotional tension and disappear during sleep. Dysarthria occurs and is often severe.
Ataxic CP is rare and results from involvement of the cerebellum or its pathways. Weakness, incoordination, and intention tremor cause unsteadiness, a wide-based gait, and difficulty with rapid or fine movements.
Mixed CP is common—most often with spasticity and athetosis.
A tool called the Gross Motor Function Classification System–Expanded and Revised (GMFCS–E&R) can be used to describe the gross motor function of children with CP. The system categorizes gross motor function into 5 different groups. It provides a description of current motor function that helps identify current and future needs for mobility aids.
Findings associated with cerebral palsy
About 25% of patients, most often those with spasticity, have other manifestations. Strabismus and other visual defects may occur. Children with athetosis due to kernicterus commonly have nerve deafness and upward gaze paralysis.
Many children with spastic hemiplegia or diplegia have normal intelligence; children with spastic quadriplegia or mixed CP may have severe intellectual disability.
Symptoms and signs references
1. Wimalasundera N, Stevenson VL: Cerebral palsy. Pract Neurol 16(3):184–194, 2016. doi: 10.1136/practneurol-2015-001184
2. Monbaliu E, Himmelmann K, Lin JP, et al: Clinical presentation and management of dyskinetic cerebral palsy. Lancet Neurol 16(9):741–749, 2017. doi: 10.1016/S1474-4422(17)30252-1
Diagnosis of Cerebral Palsy
Brain MRI
Sometimes testing to exclude hereditary metabolic or neurologic disorders
If CP is suspected, identifying the underlying disorder is important. History may suggest a cause. A brain MRI can detect abnormalities in most cases.
CP can rarely be confirmed during early infancy, and the specific type often cannot be characterized until 2 years of age. High-risk children (eg, those with evidence of asphyxia, stroke, periventricular abnormalities seen on cranial ultrasonography in preterm infants, jaundice, meningitis, neonatal seizures, hypertonia, hypotonia, or reflex suppression) should be followed closely.
Differential diagnosis
CP should be differentiated from progressive hereditary neurologic disorders and disorders requiring surgical or other specific neurologic treatments.
Ataxic CP is particularly hard to distinguish, and in many children with persistent ataxia, a progressive cerebellar degenerative disorder is ultimately identified as the cause.
Athetosis, self-mutilation, and hyperuricemia in boys indicate Lesch-Nyhan syndrome.
Cutaneous or ocular abnormalities may indicate tuberous sclerosis complex, neurofibromatosis, ataxia-telangiectasia, von Hippel–Lindau disease, or Sturge-Weber syndrome.
Infantile spinal muscular atrophy, muscular dystrophies, and neuromuscular junction disorders associated with hypotonia and hyporeflexia usually lack signs of cerebral disease.
Adrenoleukodystrophy begins later in childhood, but other leukodystrophies begin earlier and may be mistaken for CP at first.
Identification of a cause
When history and/or brain MRI does not clearly identify a cause, laboratory tests should be done to exclude certain progressive storage disorders that involve the motor system (eg, Tay-Sachs disease, metachromatic leukodystrophy, mucopolysaccharidoses) and metabolic disorders (eg, organic or amino acid metabolism disorders).
Other progressive disorders (eg, infantile neuroaxonal dystrophy) may be suggested by nerve conduction studies and electromyography. These and many other brain disorders that cause CP (and other manifestations) are being increasingly identified with genetic testing (eg, microarray analysis, CP spectrum disorders gene panel, whole exome sequencing analysis), which may be done to check for a specific disorder or to screen for many disorders.
Treatment of Cerebral Palsy
Physical and occupational therapy
Braces, constraint therapy, medications, or surgery to treat spasticity
Botulinum toxin injections
Intrathecal baclofen
Assistive devices
Physical therapy and occupational therapy for stretching, strengthening, and facilitating good movement patterns are usually used first and are continued. Bracing, constraint therapy, and medications may be added.
Botulinum toxin may be injected into muscles to decrease their uneven pull at joints and to prevent fixed contractures.
Baclofen, benzodiazepines (eg, diazepam), tizanidine, and sometimes dantrolene may diminish spasticity. Intrathecal baclofen (via subcutaneous pump and catheter) is the most effective treatment for severe spasticity. Baclofen, benzodiazepines (eg, diazepam), tizanidine, and sometimes dantrolene may diminish spasticity. Intrathecal baclofen (via subcutaneous pump and catheter) is the most effective treatment for severe spasticity.
Orthopedic surgery (eg, muscle-tendon release or transfer) may help reduce restricted joint motion or misalignment. Selective dorsal rhizotomy, done by neurosurgeons, may help a few children if spasticity affects primarily the legs and if cognitive abilities are good.
When intellectual limitations are not severe, children may attend mainstream classes and take part in adapted exercise programs and even competition. Speech training or other forms of facilitated communication may be needed to enhance interactions.
Some severely affected children can benefit from training in activities of daily living (eg, washing, dressing, feeding), which increases their independence and self-esteem and greatly reduces the burden for family members or other caregivers. Assistive devices may increase mobility and communication, help maintain range of motion, and help with activities of daily living. Some children require varying degrees of lifelong supervision and assistance.
Many children's facilities are establishing transition programs for patients as they become adults and have fewer supports to help with special needs.
Parents of a child with chronic limitations need assistance and guidance in understanding the child’s status and potential and in dealing with their own feelings of guilt, anger, denial, and sadness (see Effects on the family). These children reach their maximal potential only with stable, consistent parental care and the assistance of public and private agencies (eg, community health agencies, vocational rehabilitation organizations, lay health organizations such as United Cerebral Palsy).
Prognosis for Cerebral Palsy
Most children survive to adulthood. Severe limitations in sucking and swallowing, which may require feeding by gastrostomy tube, decrease life expectancy.
The goal is for children to develop maximal independence within the limits of their motor and associated deficits. With appropriate management, many children, especially those with spastic diplegia or hemiplegia, can lead near-normal lives.
Key Points
Cerebral palsy (CP) is a group of conditions (not a specific disorder) that involve nonprogressive spasticity, ataxia, and/or involuntary movements.
Etiology is often multifactorial and sometimes unclear but involves prenatal and perinatal factors that are associated with central nervous system (CNS) malformation or damage (eg, genetic and in utero disorders, prematurity, kernicterus, perinatal asphyxia, stroke, CNS infections).
Intellectual disability and other neurologic manifestations (eg, strabismus, deafness) are not part of CP but may be present depending on the cause.
Symptoms manifest before 2 years of age; later onset of similar symptoms suggests another neurologic disorder.
Do brain MRI and, if needed, testing for hereditary metabolic and neurologic disorders.
Treatment depends on the nature and degree of disability, but physical therapy and occupational therapy are typically used; some children benefit from bracing, botulinum toxin, benzodiazepines, other muscle relaxants, intrathecal baclofen, and/or surgery (eg, muscle-tendon release or transfer, rarely dorsal rhizotomy).Treatment depends on the nature and degree of disability, but physical therapy and occupational therapy are typically used; some children benefit from bracing, botulinum toxin, benzodiazepines, other muscle relaxants, intrathecal baclofen, and/or surgery (eg, muscle-tendon release or transfer, rarely dorsal rhizotomy).
More Information
The following English-language resources may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
CanChild: Gross Motor Function Classification System–Expanded and Revised (GMFCS–E&R): A tool for describing the gross motor function of children with CP (available in many languages)
United Cerebral Palsy: Provides information about therapy, early intervention programs, and support services for people who have cerebral palsy and other disabilities